Etiology
Mycobacterium tuberculosis
- Virulence factors and resistances
- Cord factor: arranges M. tuberculosis in a serpentine cord → ↑ TNF-α release and activation of macrophages → granuloma formation
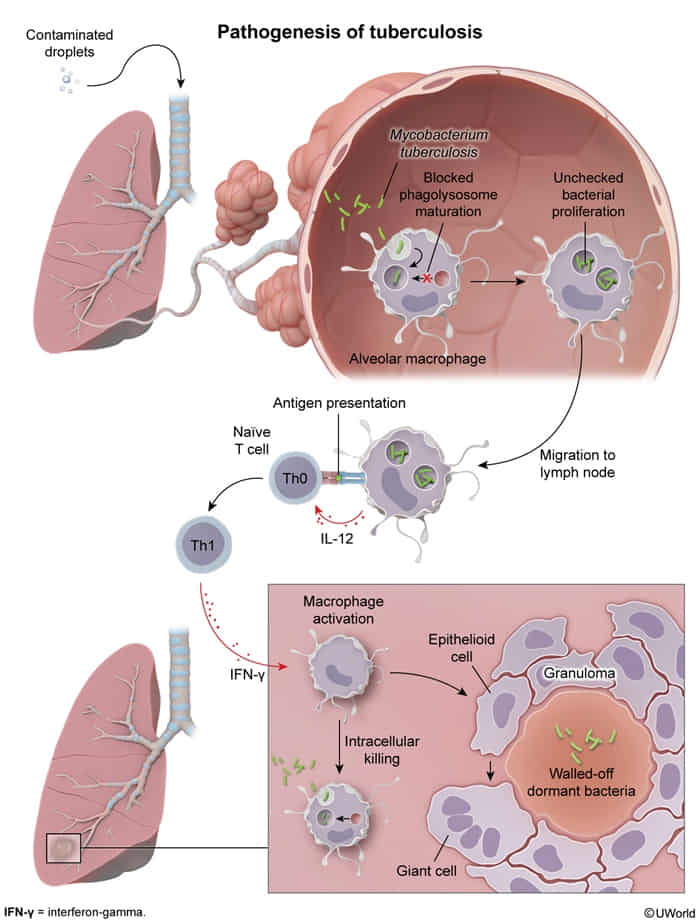
- Surface glycolipids: (sulfatides) inhibit phagolysosomal fusion
- Infiltration of nonactivated macrophages → escape of humoral immune response
- Multi-drug resistance: mutation in KatG (catalase-peroxidase) → INH conversion to its active metabolite → INH resistance
- Cord factor: arranges M. tuberculosis in a serpentine cord → ↑ TNF-α release and activation of macrophages → granuloma formation
Pathophysiology
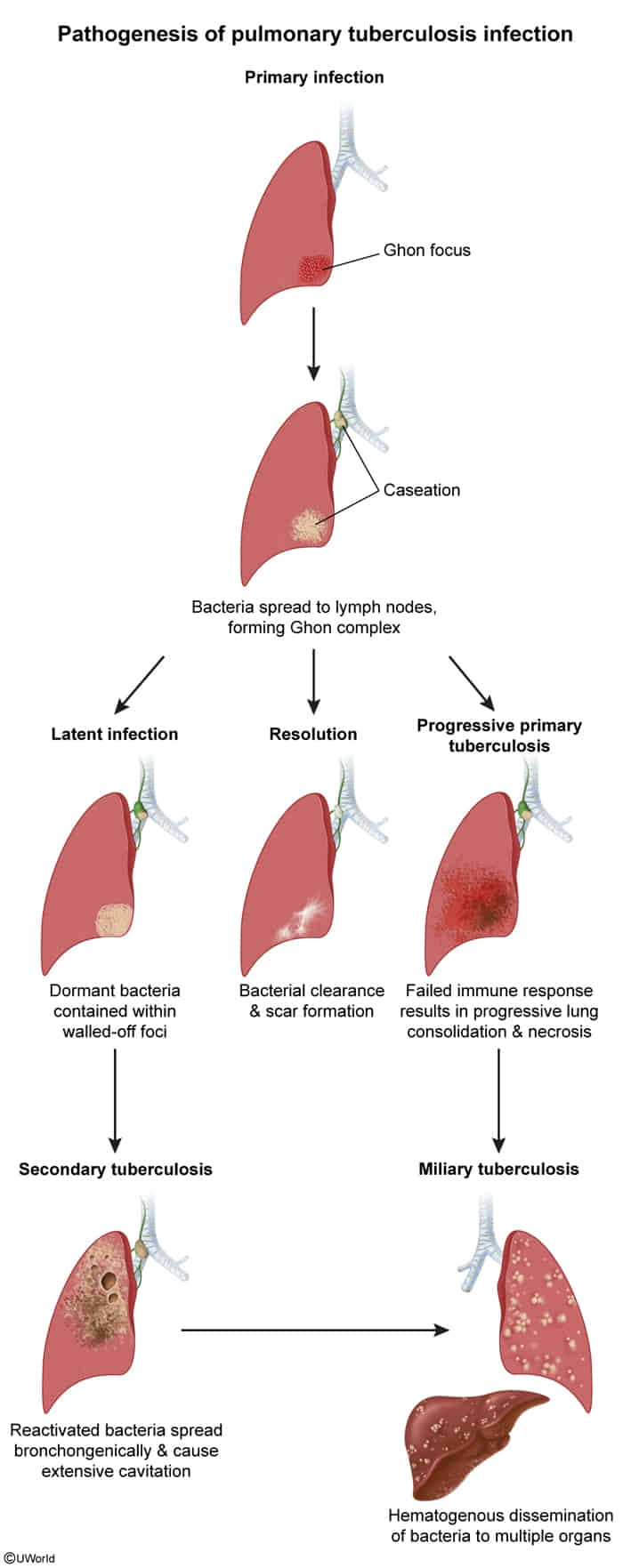
Primary tuberculosis
- Ghon focus: a granuloma typically located in the middle/lower lung lobes.
- Ghon complex: formed by the Ghon focus, regional lymph node, and the linking lymphatic vessels
- The organisms can remain dormant in a walled-off Ghon complex for many years before reactivating.
- Alternatively, the lesion may heal, forming a benign, calcified Ranke complex that is not associated with reactivation tuberculosis.
Secondary tuberculosis
- In < 10% of individuals with primary TB, the host immune response fails to control the infection, leading to active primary TB and progressive disease.
- In > 90% of individuals, the host immune response can control the infection, resulting in latent TB infection. Weakening of host immune response can allow reactivation of disease (or, less commonly, reinfection) and further disease progression.
Clinical features
Diagnostics
Active TB infection
- Acid-fast bacilli smear microscopy
- Description: Ziehl Neelsen stain or auramine rhodamine stain are used.
- Advantages:
- Rapid detection
- Inexpensive
- Disadvantages:
- Low sensitivity
- Cannot differentiate M. tuberculosis from other nontuberculous mycobacteria
- Both viable and nonviable mycobacteria will stain
- Nucleic acid amplification test
- Description: For initial testing (along with AFB smear microscopy and culture) if clinical suspicion is high. Used for confirmation of AFB positive smears.
- Advantages:
- High specificity and sensitivity (lower sensitivity in individuals with a negative AFB smear)
- Rapid diagnosis
- Rapid detection of drug-resistant strains
- Low cross-reactivity with nontuberculous mycobacteria
- Disadvantages:
- Requires laboratory equipment and trained staff, which may make use in resource-limited settings more difficult
- Both viable and nonviable mycobacteria are detectable
- Culture
Latent TB infection
- Tuberculin skin test (purified protein derivative test, Mantoux test)
- Mechanism
- Tests cell-mediated immunity against M. tuberculosis via delayed hypersensitivity reaction (type IV HSR) mounted by T cells
- Does not differentiate between active and latent TB
- False positives resulting from either of the following:
- Prior BCG vaccination
- Exposure to nontuberculous mycobacteria
- False negatives are possible in patients with any of the following:
- Sarcoidosis
- Immunosuppressed state (anergy)
- Mechanism
- Interferon-γ release assay (IGRA)
- Mechanism
- Tests cell-mediated immunity against M. tuberculosis-specific antigens by measuring the amount of IFN-γ released by T cells using ELISA
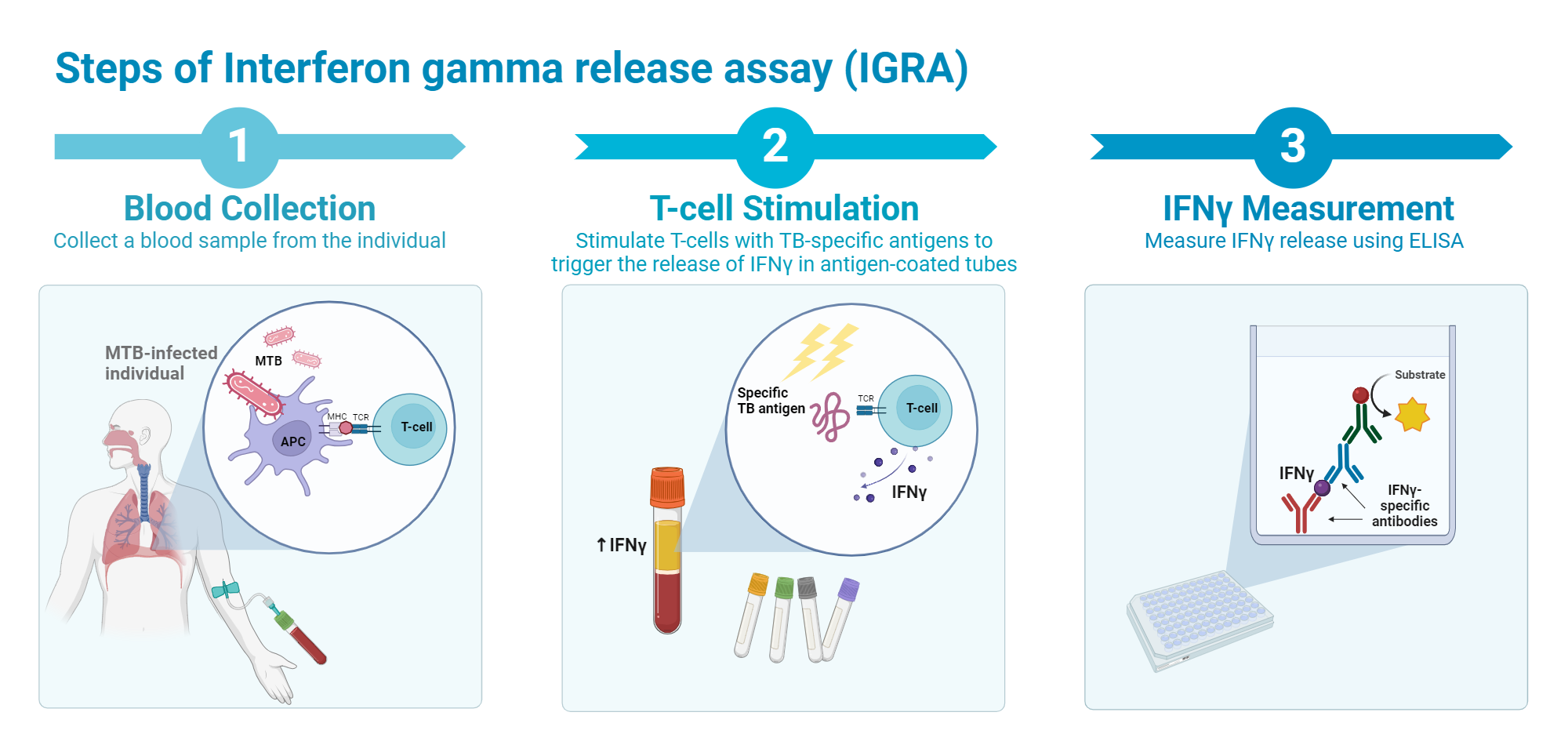
- Tests cell-mediated immunity against M. tuberculosis-specific antigens by measuring the amount of IFN-γ released by T cells using ELISA
- Preferred test in individuals with prior BCG vaccination
- Uses antigens that are found only in Mycobacterium tuberculosis, but not in BCG
- Mechanism
Extrapulmonary tuberculosis
- General: May present with constitutional “B” symptoms (fever, night sweats, weight loss) or be asymptomatic.
- Lymphadenitis (Scrofula): Most common form. Presents as chronic, painless, “cold” abscess, typically in the cervical or supraclavicular nodes. May form a draining fistula with caseous material.
- Pleural TB: Common form, often from rupture of a subpleural focus. Presents with pleuritic chest pain and dyspnea. Pleural effusion is exudative with high protein, high lymphocytes, and often low glucose and high adenosine deaminase (ADA).
- Skeletal (Pott Disease): Involves the spine, especially the thoracic vertebrae. Presents with chronic back pain, tenderness, and may lead to vertebral collapse, kyphosis (gibbus), and paraspinal “cold” abscesses.
- Genitourinary (GU) TB: Affects kidneys, bladder, and genitalia. Presents with sterile pyuria (WBCs in urine without bacteria on standard culture), hematuria, and flank pain. Can cause infertility.
- CNS (Tuberculous Meningitis): Most severe form. Occurs at the base of the brain, leading to cranial nerve palsies (e.g., CN III, VI). Presents with subacute headache, fever, and nuchal rigidity. CSF shows high lymphocytes, very high protein, and low glucose.
- Gastrointestinal TB: Ileocecal region is the most common site. Can mimic Crohn’s disease, causing abdominal pain, diarrhea, and a right lower quadrant mass.
- Pericardial TB: Can cause pericardial effusion, tamponade, or constrictive pericarditis.
- Miliary TB: Disseminated disease from hematogenous spread, resulting in millet-seed-like lesions in multiple organs (liver, bone marrow, spleen, lungs).
Treatment
Mnemonic
b在里,脸在外,利益万能,纯洁无害
- 吡 细胞内
- 链 细胞外
- 利 内+外
- 醇 抑菌不杀菌
Rifamycins
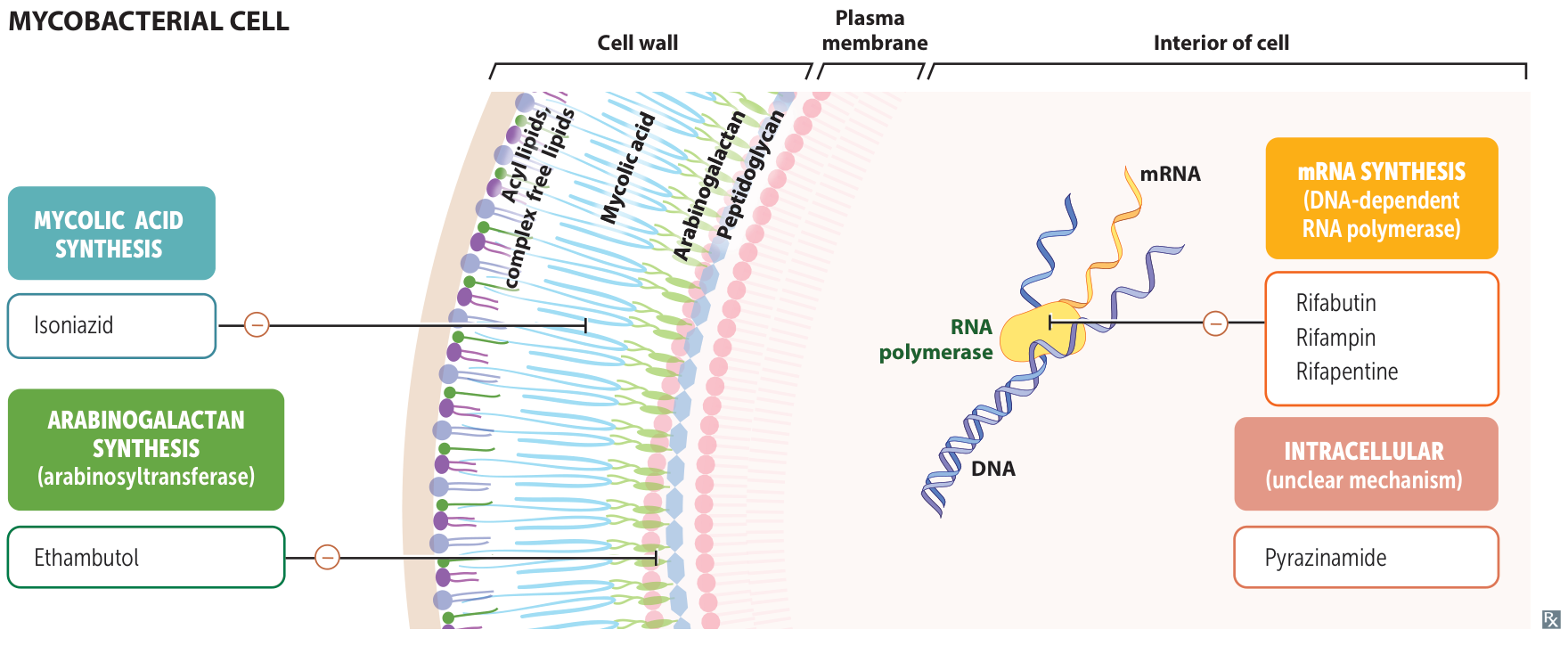
- Mechanism of action: inhibits bacterial DNA-dependent RNA-polymerase → prevention of transcription (mRNA synthesis) → inhibition of bacterial protein synthesis → cell death (bactericidal effect) t
- Mnemonic: “R for RNA Polymerase.”
- Other uses
- Prophylaxis:
- Meningococcal (N. meningitidis) contacts. t
- H. influenzae type b contacts.
- Prophylaxis:
Isoniazid (INH)
- Mechanism of action
- Isoniazid is a prodrug and needs to be converted into its active metabolite by bacterial catalase-peroxidase (encoded by KatG). t
- Prevents cell wall synthesis by inhibiting the synthesis of mycolic acid
- Mnemonic: “INHibits mycolic acid synthesis.”
Pyrazinamide
- Mechanism of action
- Not completely understood
- Prodrug: converted into active form pyrazinoic acid
- Most effective at acidic pH (e.g., in acidic phagolysosomes)
- Bactericidal effect
- Not completely understood
Ethambutol
- Mechanism of action: inhibits arabinosyltransferase → ↓ carbohydrate polymerization → prevention of mycobacterial cell wall synthesis (bacteriostatic effect)
Side effects of antituberculosis agents
- Isoniazid
- Asymptomatic elevation of transaminases
- In 10%-20% of patients, INH causes acute, mild hepatic dysfunction
- In rare instances (<1%), INH induces a frank hepatitis that causes a syndrome similar to viral hepatitis (eg, fever, anorexia, nausea, jaundice) t
- Cytochrome P450 inhibition: leading to interactions with numerous drugs, including antiretroviral agents, cardiovascular agents, and antibiotics
- Less common
- Drug-induced lupus
- Vitamin B6 deficiency: sideroblastic anemia, peripheral neuropathy t
- Isoniazid is structurally similar to pyridoxine (vitamin B6), a cofactor for enzymes involved in synthesis of certain neurotransmitters. Because of this similarity, isoniazid acts as a competitive inhibitor of pyridoxine and can cause dose-related peripheral neuropathy (eg, numbness and tingling in the hands and feet).
- CNS toxicity: precipitation of benzodiazepine-refractory seizures with high doses of isoniazid, psychosis, ataxia
- Others: anion gap metabolic acidosis, pellagra, optic neuritis
- Asymptomatic elevation of transaminases
- Rifampin
- Cytochrome P450 induction: leading to important interactions with ART in patients with HIV (therefore, rifabutin is preferred)
- Orange discoloration of body fluids
- Pyrazinamide
- Greatest hepatotoxicity potential
- Hyperuricemia
- Ethambutol
- Optic neuritis (reversible red-green color blindness)