Function
Mnemonic
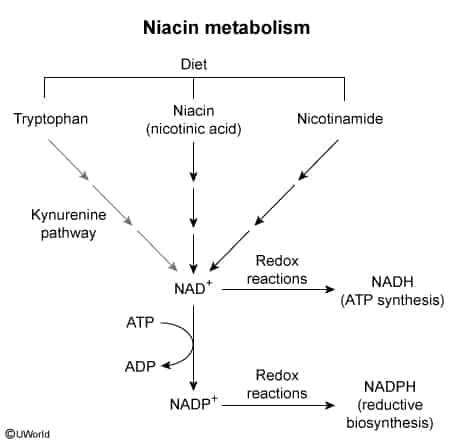
Active forms of Niacin are NAD+ and NADP+.
- Cofactor for redox reactions (e.g., alcohol dehydrogenase, isocitrate dehydrogenase, G6PD)
- Required for the metabolism of fats, carbohydrates, and proteins.
- Synthesized endogenously from the amino acid tryptophan. Requires vitamins B2 (riboflavin) and B6 (pyridoxine) as cofactors.
Therapeutic use
- Dyslipidemia: Niacin lowers VLDL and increases HDL serum levels (See Lipid-lowering agents)
Vitamin B3 deficiency
Etiology
- Malnutrition: Most common cause worldwide (e.g., alcohol use disorder, diets heavy in corn).
- Hartnup disease: Autosomal recessive disorder causing defective intestinal and renal absorption of neutral amino acids, including tryptophan. t
- Malignant carcinoid syndrome: Increased metabolism of tryptophan to serotonin leads to less tryptophan available for niacin synthesis.
- Isoniazid (INH) therapy: INH depletes vitamin B6 (pyridoxine), a required cofactor for niacin synthesis.
- Prolonged diarrhea: Malabsorption.
Pathophysiology
Clinical features (Pellagra)
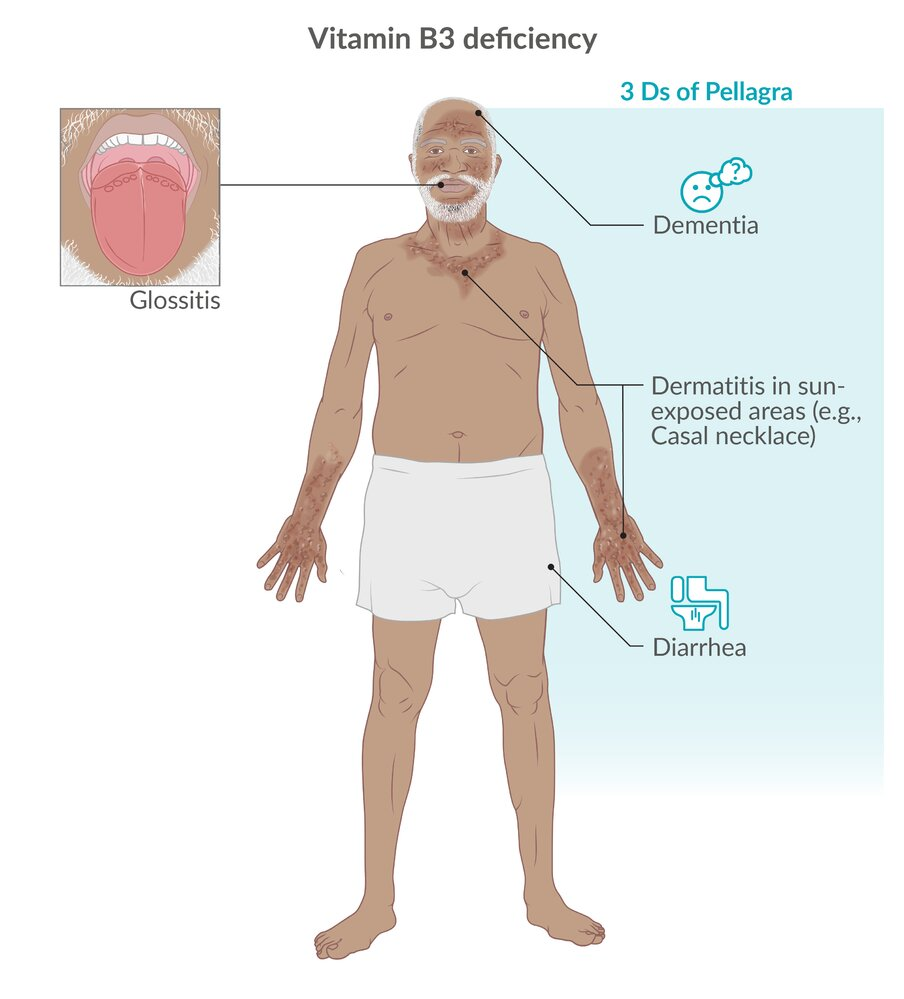
- Dermatitis:
- Photosensitive hyperpigmented rash on sun-exposed areas. t
- Casal necklace: Broad collar-like rash on the neck (C3/C4 dermatome).
- Thick, scaly skin on hands/feet (“glove and stocking”).

- Diarrhea: Atrophy of columnar epithelium of GI tract.
- Dementia: Neuronal degeneration (hallucinations, insomnia, anxiety, memory loss).
- Glossitis: Swollen, beefy-red tongue.
Mnemonic
Diagnostics
Treatment
Vitamin B3 toxicity
- Facial flushing: due to prostaglandin release and NOT due to histamine (typically seen when niacin therapy is started, can be avoided by coadministration of aspirin)
- Hyperuricemia, podagra
- Niacin decreases renal uric acid excretion.
- Hyperglycemia