Etiology
- PBC is considered an autoimmune disease
- Often associated with other autoimmune conditions, e.g.:
- CREST syndrome
- Sicca syndrome
- Autoimmune thyroid disease, especially Hashimoto thyroiditis
- Celiac disease
- Rheumatoid arthritis
Pathophysiology
Inflammation and progressive destruction (likely due to an autoimmune reaction) of the small and medium-sized intrahepatic bile ducts (progressive ductopenia) → defective bile duct regeneration → chronic cholestasis → secondary hepatocyte damage due to increased concentration of toxins that typically get excreted via bile → gradual portal and periportal fibrotic changes → liver failure → liver cirrhosis and portal hypertension (in advanced stage)
Clinical features
Clinical features of PBC
Similar to PSC + xanthomas and xanthelasma
Patients with PBC are usually initially asymptomatic.
- Fatigue: most common and often the first symptom
- Marked pruritus: generalized
- Symptoms of cholestasis
- Jaundice
- Pale stool, dark urine
- Maldigestion (more common in advanced disease)
- Deficiency of fat-soluble vitamins (A, D, E, and K)
- Signs of cirrhosis and portal hypertension
- Hepatomegaly with dull lower margin, RUQ discomfort
- Splenomegaly
- Hyperpigmentation
- Due to increased amounts of melanin; the exact cause and pathomechanism remain unclear.
- Xanthomas and xanthelasma
Diagnostics
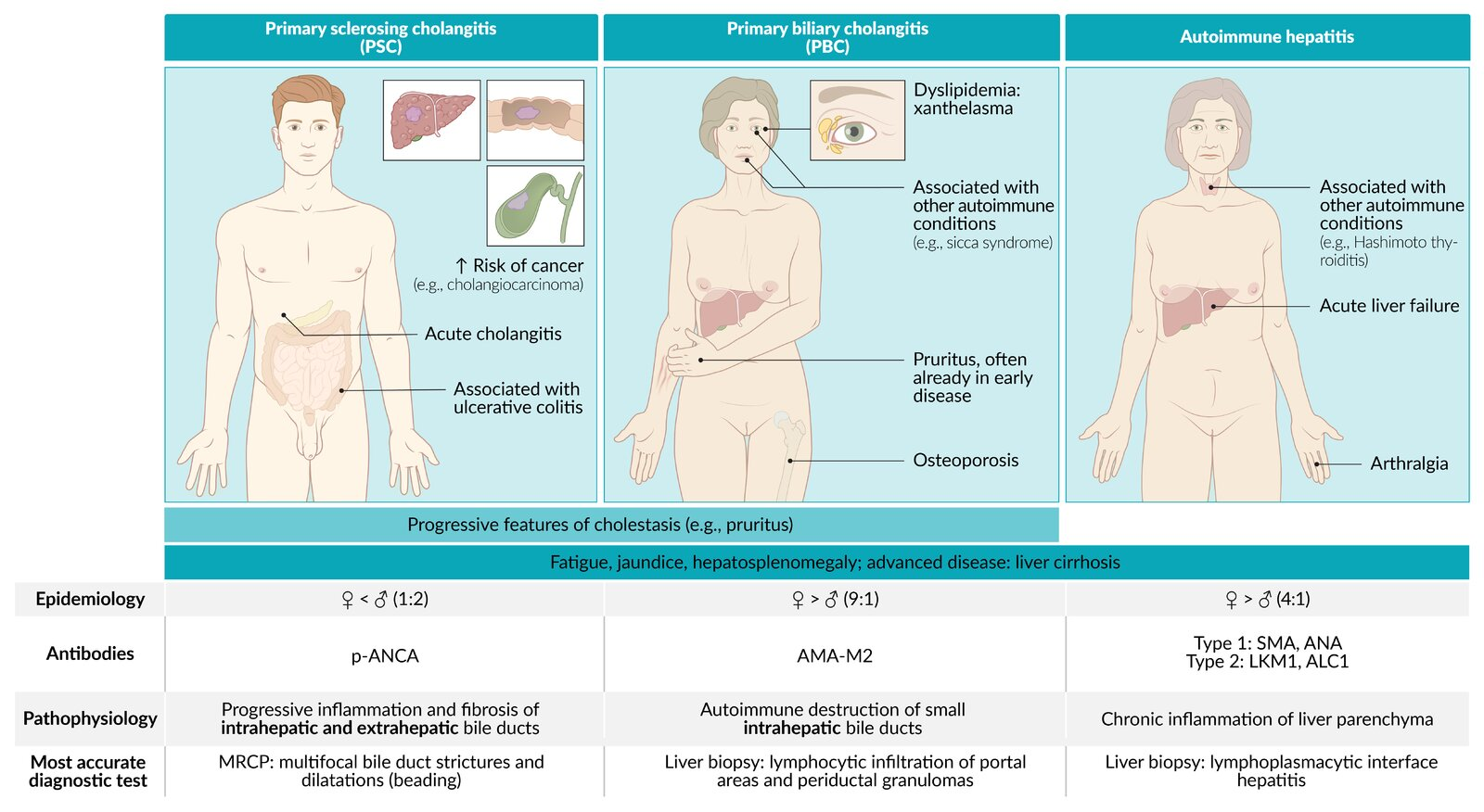
Autoimmune Liver Diseases
Mnemonic
- PBC: Boobs, Women get it (autoimmune + mitochondria from mom) → “Women stay inside” (intrahepatic ducts only).
- PSC: Scrotom, Men get it → “Men go wherever” (intra- and extrahepatic ducts) + p-ANCA (“perineuclear” → crude link to male anatomy).
Feature Primary Sclerosing Cholangitis (PSC) Primary Biliary Cholangitis (PBC) Autoimmune Hepatitis (AIH) Patho Inflammation/fibrosis of intra- & extrahepatic bile ducts Autoimmune destruction of intrahepatic bile ducts Autoimmune destruction of hepatocytes Epi / Assoc. M > F (2:1), <40s
Assoc: Ulcerative Colitis (IBD) (>80%)F >> M (9:1), 40-60s
Assoc: Sjögren’s, other autoimmune dzF > M (3:1), bimodal (young/middle-aged)
Assoc: Other autoimmune dzLabs Cholestatic: ↑↑ ALP, ↑ GGT Cholestatic: ↑↑ ALP, ↑ GGT Hepatocellular: ↑↑↑ AST/ALT (>1000s common), ↑ IgG Serology (+) p-ANCA (+) AMA (Anti-Mitochondrial Ab) (+) ANA, (+) ASMA (Anti-Smooth Muscle Ab) Dx / Histo MRCP/ERCP: “Beads on a string”
Histo: “Onion skinning” periductal fibrosisNormal imaging
Histo: Florid duct lesion (lymphocytic cholangitis, granulomas)Normal/nonspecific imaging
Histo: Interface hepatitis, plasma cellsTx Symptomatic Tx; Liver transplant (definitive) Ursodeoxycholic acid (UDCA) Corticosteroids, Azathioprine Key Risk Cholangiocarcinoma, Colorectal Cancer (w/ UC) Osteoporosis, Cirrhosis, HCC Cirrhosis, Acute Liver Failure Link to original
- Liver chemistries: cholestatic pattern of injury
- ↑ ALP, ↑ GGT, ↑ direct bilirubin
- Mild transaminitis (or normal AST and ALT)
- Lipid panel: hypercholesterolemia
- PBC-specific autoantibodies
- Antimitochondrial antibodies (AMA) (present in > 95% of patients)
- Immunoglobulins (nonspecific)
- ↑ IgM
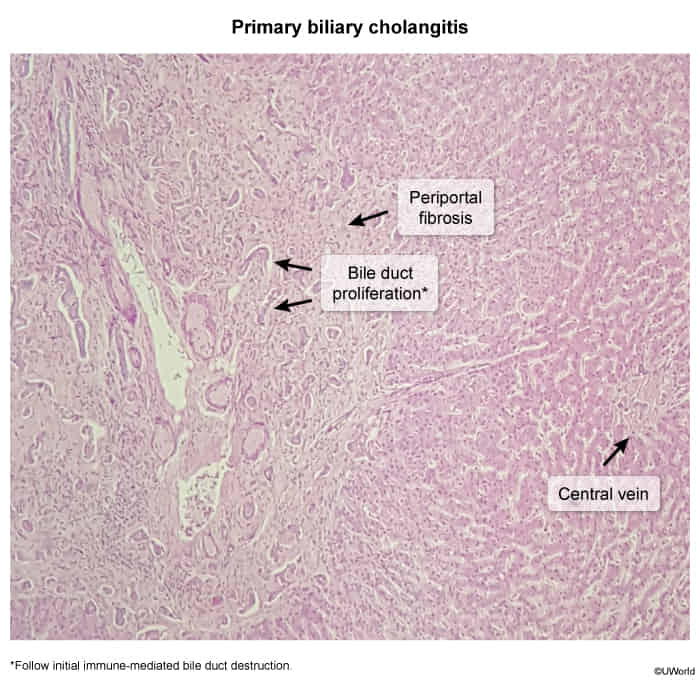
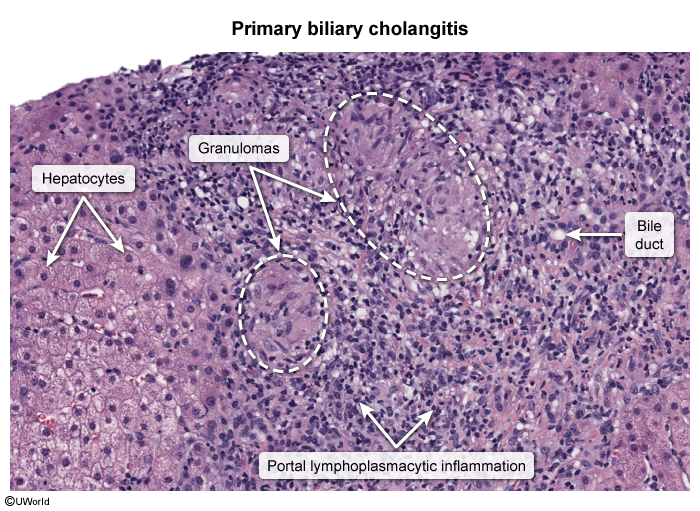
- Biopsy
- Florid Duct Lesion: Granulomatous destruction of bile ducts.
- Non-caseating granulomas in the portal triad.
Treatment
General principles
- Start pharmacotherapy with ursodeoxycholic acid for all patients.
- Offer supportive care, including management of cholestasis-associated pruritus.
- Liver transplantation is necessary if liver cirrhosis is advanced.
Pharmacotherapy
- First-line: ursodeoxycholic acid (UDCA, ursodiol): a hydrophilic, nontoxic bile acid
- Mechanism
- Normal bile acid is hydrophobic. When bile ducts are blocked (as in PBC), these bile acids back up and start dissolving the membranes of the liver cells. When you take Ursodiol, it enters your system and eventually replaces up to 50% of the bile pool. It dilutes the “toxic” bile, making the mixture much less corrosive.
- ↓ Cholesterol secretion into bile; makes bile less lithogenic.
- Dissolves cholesterol stones.
- Indications
- Primary Biliary Cholangitis (PBC): First-line therapy (delays progression).
- Gallstones: Medical dissolution of radiolucent (cholesterol) stones in poor surgical candidates.
- Rapid weight loss: Prophylaxis against stone formation.
- Adverse Effects
- Diarrhea.
- Mechanism