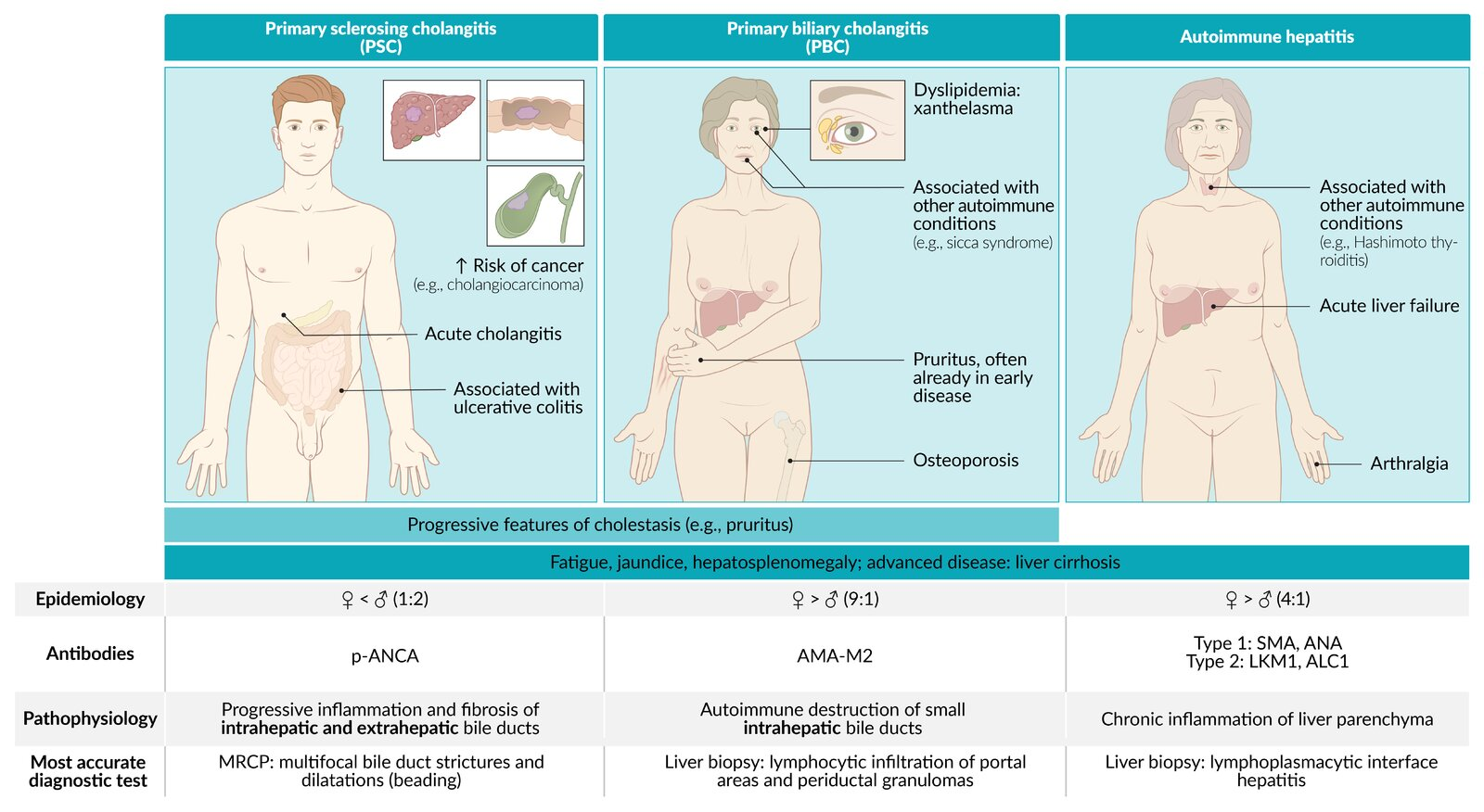
Epidemiology
- Sex: ♂ > ♀ (2:1)
- Age: The median age at diagnosis is ∼ 40.
Tip
Compared with Primary biliary cholangitis, which are common among middle-aged women.
Etiology
- The exact cause is unknown.
- Associations
- Chronic inflammatory bowel diseases (IBD)
- ∼ 90% of patients with PSC have IBD (approx. 87% of these patients have ulcerative colitis)
- Presence of HLA-B8 and HLA-DR3
- Chronic inflammatory bowel diseases (IBD)
The majority of patients with PSC also have
Pathophysiology
Progressive chronic inflammation of both intrahepatic and extrahepatic bile ducts
Clinical features
- Signs of cholestasis
- Jaundice/scleral icterus
- Pruritus
- Pale stool, dark urine
- Fatigue
- Can lead to acute cholangitis (fever, chills, right upper quadrant pain)
- Later stages: signs of cirrhosis
- Hepatosplenomegaly
- Portal hypertension
- Liver failure
- Symptoms of chronic inflammatory bowel disease, which is frequently associated with PSC, or other associated comorbidities
Diagnostics
Autoimmune Liver Diseases
Mnemonic
- PBC: Boobs, Women get it (autoimmune + mitochondria from mom) → “Women stay inside” (intrahepatic ducts only).
- PSC: Scrotom, Men get it → “Men go wherever” (intra- and extrahepatic ducts) + p-ANCA (“perineuclear” → crude link to male anatomy).
Feature Primary Sclerosing Cholangitis (PSC) Primary Biliary Cholangitis (PBC) Autoimmune Hepatitis (AIH) Patho Inflammation/fibrosis of intra- & extrahepatic bile ducts Autoimmune destruction of intrahepatic bile ducts Autoimmune destruction of hepatocytes Epi / Assoc. M > F (2:1), <40s
Assoc: Ulcerative Colitis (IBD) (>80%)F >> M (9:1), 40-60s
Assoc: Sjögren’s, other autoimmune dzF > M (3:1), bimodal (young/middle-aged)
Assoc: Other autoimmune dzLabs Cholestatic: ↑↑ ALP, ↑ GGT Cholestatic: ↑↑ ALP, ↑ GGT Hepatocellular: ↑↑↑ AST/ALT (>1000s common), ↑ IgG Serology (+) p-ANCA (+) AMA (Anti-Mitochondrial Ab) (+) ANA, (+) ASMA (Anti-Smooth Muscle Ab) Dx / Histo MRCP/ERCP: “Beads on a string”
Histo: “Onion skinning” periductal fibrosisNormal imaging
Histo: Florid duct lesion (lymphocytic cholangitis, granulomas)Normal/nonspecific imaging
Histo: Interface hepatitis, plasma cellsTx Symptomatic Tx; Liver transplant (definitive) Ursodeoxycholic acid (UDCA) Corticosteroids, Azathioprine Key Risk Cholangiocarcinoma, Colorectal Cancer (w/ UC) Osteoporosis, Cirrhosis, HCC Cirrhosis, Acute Liver Failure Link to original
- Cholestatic enzymes
- ↑ ALP
- ↑ GGT
- Normal or ↑ conjugated bilirubin
- Transaminases: normal or moderately elevated (approx. 2–3× ULN) AST and ALT
- Lipid profile: ↑ total cholesterol
Mnemonic
Suspect PSC in patients with a history of inflammatory bowel disease and elevated cholestatic enzymes (ALP, GGT, and conjugated bilirubin).
- Typical perinuclear anti-neutrophil cytoplasmic antibodies (pANCA): present in up to 80% of patients with PSC.
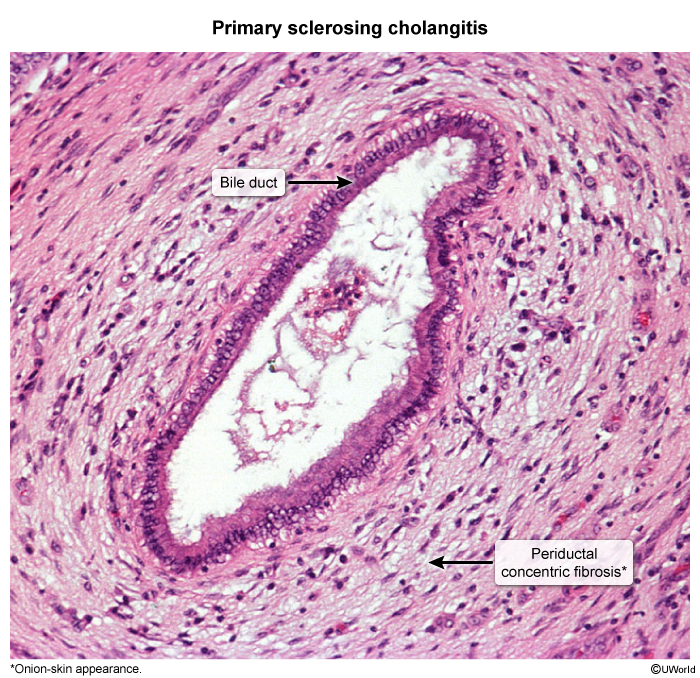
- Pathology: periductal concentric fibrosis around bile ducts → “Onion skin” appearance.
Magnetic resonance cholangiopancreatography
- Method of choice (if there is no biliary obstruction)
- Supportive findings: multifocal intrahepatic and extrahepatic bile duct strictures alternating with dilatation and beading of bile ducts
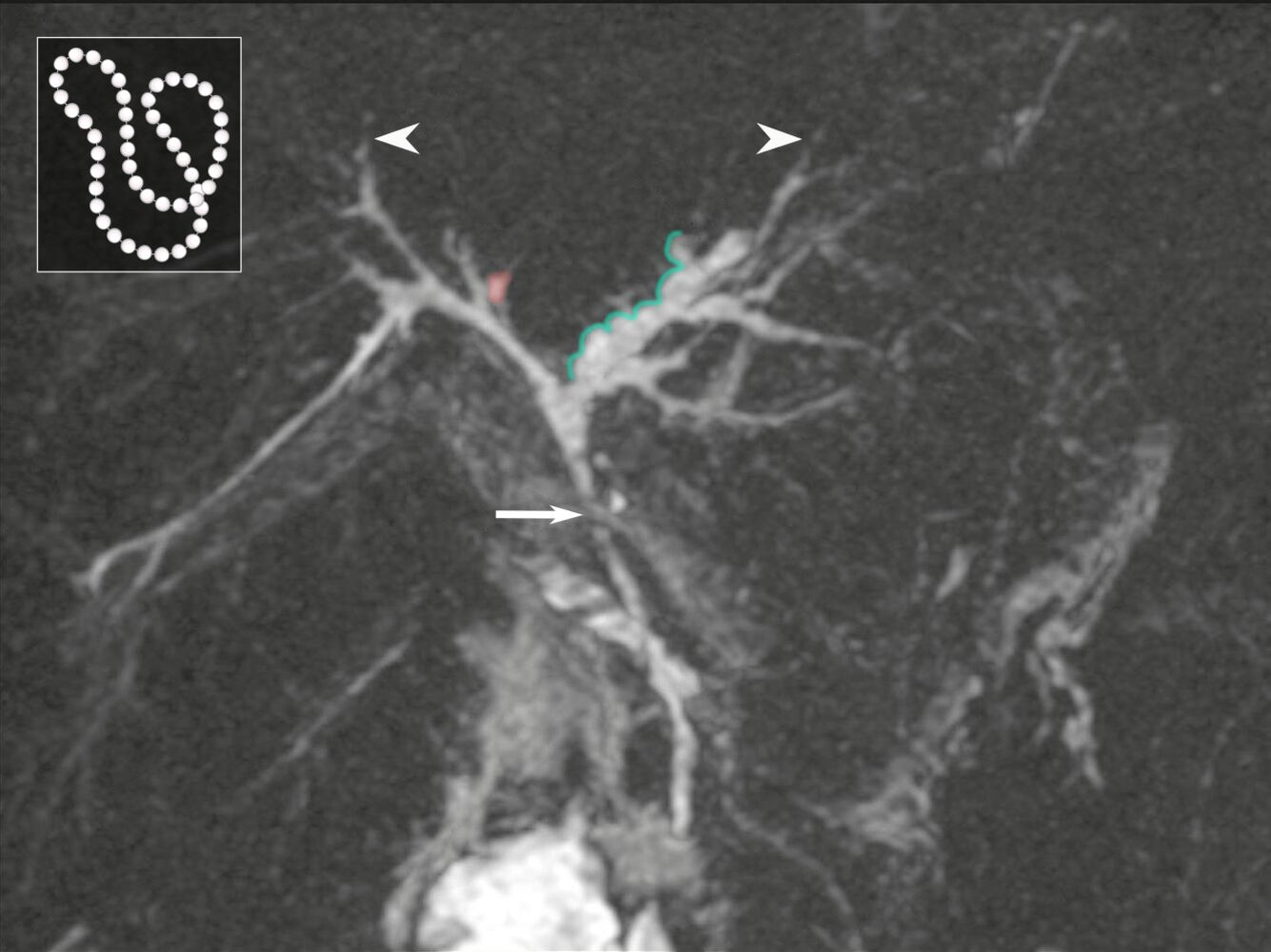 There is irregular dilatation (green overlay) of intrahepatic bile ducts proximal to a common duct stenosis (arrow). Alternation of strictured and dilated segments creates a beaded appearance. Peripheral ducts appear pruned as a result of obliteration (examples indicated by arrowheads), and scattered biliary diverticula are seen (example indicated by red overlay).
There is irregular dilatation (green overlay) of intrahepatic bile ducts proximal to a common duct stenosis (arrow). Alternation of strictured and dilated segments creates a beaded appearance. Peripheral ducts appear pruned as a result of obliteration (examples indicated by arrowheads), and scattered biliary diverticula are seen (example indicated by red overlay).
Treatment
Complications
- Cholangiocarcinoma (∼ 10–15% of cases)