Epidemiology
Etiology
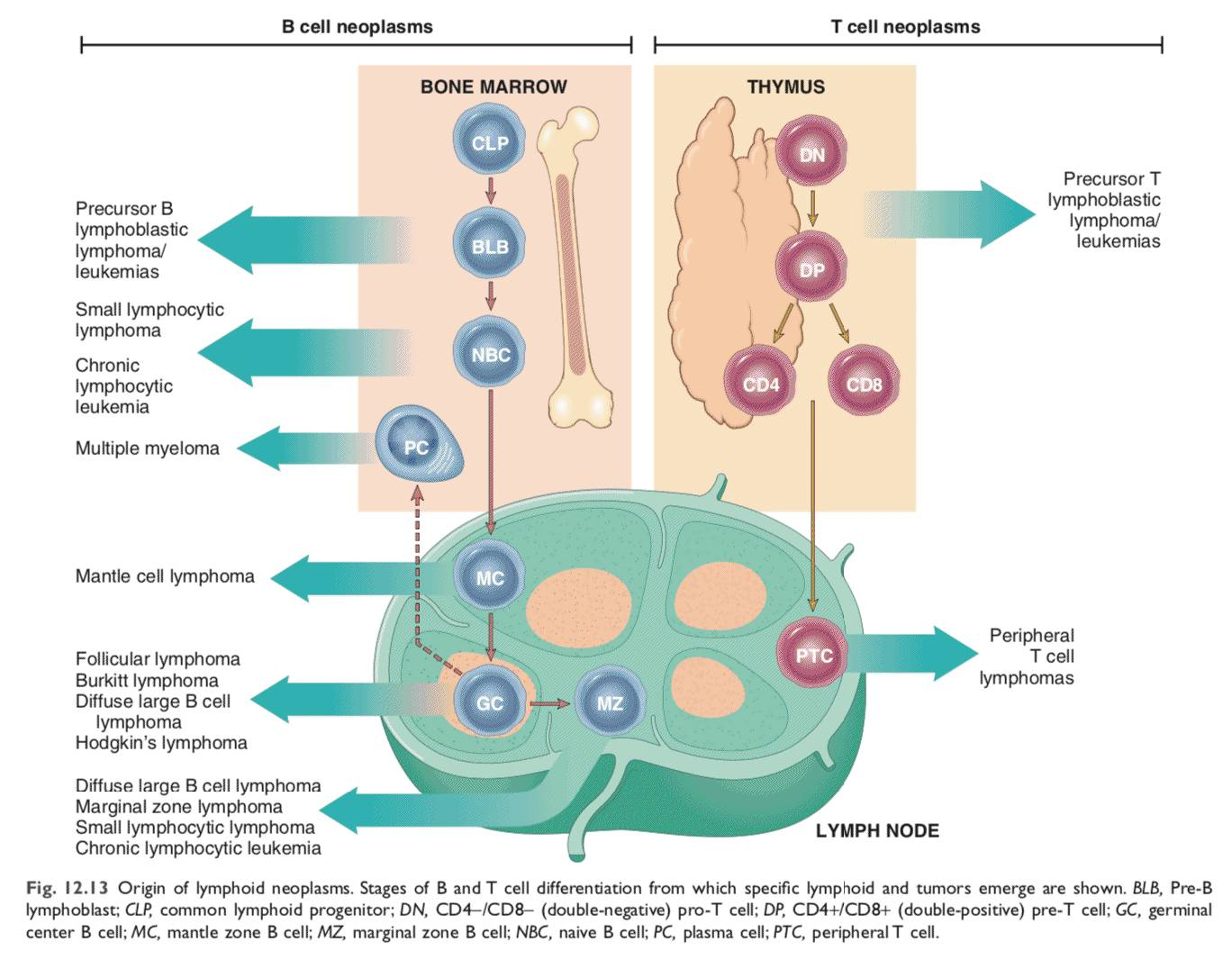
Pathophysiology
Clinical features
Indolent (low-grade)
- Follicular lymphoma
- Most common low-grade lymphoma in adults
- Slowly progressive and painless course with an alternating (waxing and waning) pattern of lymphadenopathy and splenomegaly
- Translocation t(14;18), which involves the heavy-chain Ig (chromosome 14) and Bcl-2 gene (chromosome 18) → overexpression of Bcl-2 → dysregulation of apoptosis (normally inhibited by Bcl-2)
- Centrocyte: nodular, small cells with cleaved nuclei
Aggressive (high-grade)
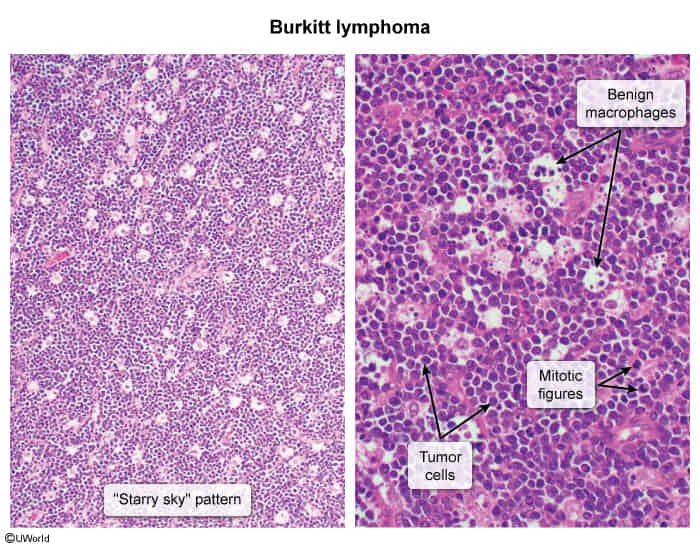
- Burkitt lymphoma
- Most common in children
- Translocation t(8;14) in 75% of cases: reciprocal translocation involving the c-myc gene (chromosome 8) and heavy-chain Ig locus (chromosome 14) → overactivation of c-myc proto-oncogene → activation of transcription
- Forms
- Sporadic: typically located in the abdomen or pelvis
- Endemic: associated with EBV (most prevalent in equatorial Africa and South America) and is typically located in the maxillary and mandibular bones t
- Immunodeficiency-associated: e.g. HIV infection
- Starry sky pattern (See below)
- Nonendemic BL often involves the gastrointestinal tract, which can present as an enlarging abdominal mass with ascites (due to lymph obstruction) and distention and obstruction.
Hodgkin lymphoma vs non-Hodgkin lymphoma
Link to original
Feature Hodgkin Lymphoma (HL) Non-Hodgkin Lymphoma (NHL) Key Cell Reed-Sternberg (“owl-eye”) Malignant lymphocytes (B or T cell) Spread Contiguous (orderly, predictable) Non-contiguous (disseminated) Presentation Localized, single node group (e.g., cervical, mediastinal) Multiple peripheral nodes, extranodal common ”B” Symptoms Common (fever, night sweats, wt loss) Less common Age Bimodal (20s, >50s) Typically >50 years old Prognosis High cure rate Variable; depends on subtype Key Associations EBV EBV, HTLV-1, HHV-8; translocations (e.g., t(14;18), t(8;14))
Diagnostics
Tip
Lymphoma arises from mature lymphocytes and often forms tumors in the lymphatic system, leukemia typically originates from immature progenitor cells in the bone marrow and is characterized by abnormal cells circulating in the blood.
Chromosomal translocations
| Malignancy | Pathogenesis |
|---|---|
| Acute promyelocytic leukemia | t(15;17) involving PML & RARA → PML-RARα oncoprotein → myeloid differentiation inhibited RARα: nuclear receptor involved in myeloid differentiation PML: fusion forms receptor with dominant negative activity |
| Burkitt lymphoma | t(8;14) involving MYC & IGH → MYC overexpression → cell growth MYC: transcription factor regulating cell growth IGH: immunoglobulin heavy chain (high expression in B cells) |
| Chronic myeloid leukemia | t(9;22) involving ABL1 & BCR → BCR-ABL1 oncoprotein → cell proliferation ABL1: nonreceptor tyrosine kinase BCR: fusion leads to activation |
| Follicular lymphoma | t(14;18) involving IGH & BCL2 → BCL2 overexpression → apoptosis evasion BCL2: antiapoptotic protein t |
| Mantle cell lymphoma | t(11;14) involving CCND1 & IGH → cyclin D1 overexpression → cell cycle progression Cyclin D1: regulates cell cycle progression |
Pathology
Only those with pictures are important
- Diffuse Large B-Cell Lymphoma (DLBCL)
- Sheets of large, atypical lymphocytes that efface the normal lymph node architecture.
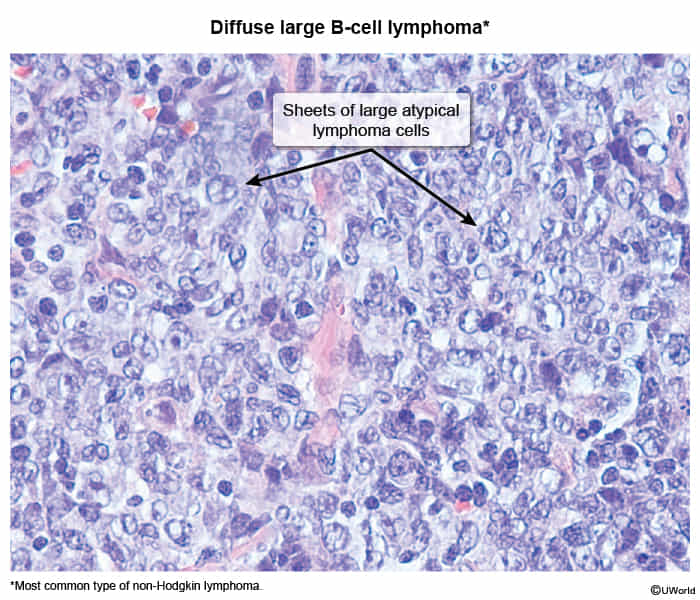
- Sheets of large, atypical lymphocytes that efface the normal lymph node architecture.
- Follicular Lymphoma
- Nodular (follicular) aggregates of small, cleaved cells (centrocytes) and large cells (centroblasts).
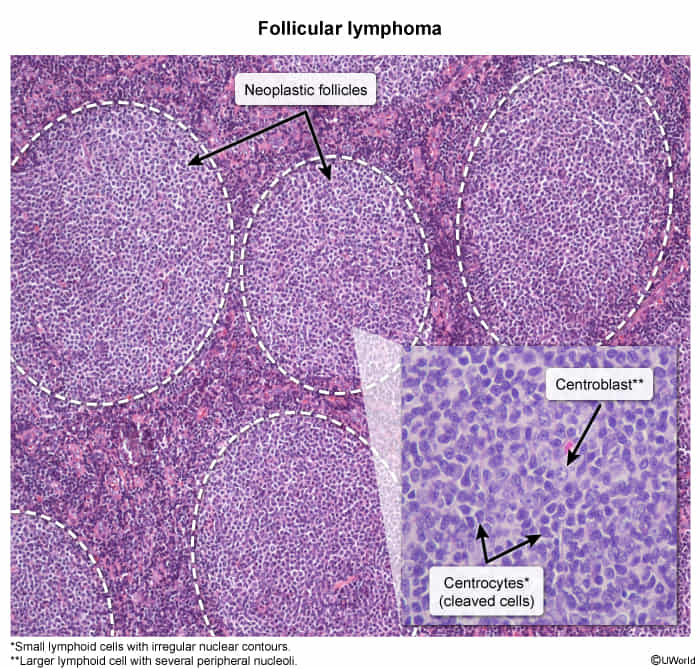
- Nodular (follicular) aggregates of small, cleaved cells (centrocytes) and large cells (centroblasts).
- Mantle Cell Lymphoma
- Monotonous population of small to medium-sized lymphocytes expanding the mantle zone around germinal centers.
- Burkitt Lymphoma
- Diffuse infiltrate of medium-sized lymphocytes with a high mitotic rate and apoptotic bodies (not necrosis), creating a “starry sky” appearance. t
- Tingible body macrophages (containing many phagocytized tumor cells) are scattered diffusely within a sheet of uniform neoplastic cells (lymphocytes).
- The dark sky is malignant lymphocytes, the stars are benign tangible-body macrophages.
- Marginal Zone Lymphoma
- Infiltration of the marginal zone of lymphoid follicles, often seen in mucosa-associated lymphoid tissue (MALT).
- Small Lymphocytic Lymphoma (SLL)
- Diffuse effacement of lymph node architecture by small, mature-appearing lymphocytes. “Smudge cells” are a characteristic finding on slide preparations.
- Adult T-Cell Leukemia/Lymphoma (ATLL)
- Presence of atypical T-cells with multi-lobed, “flower-like” nuclei.
- Mycosis Fungoides / Sézary Syndrome
- Infiltration of the epidermis by atypical T-cells with convoluted, cerebriform nuclei, which can form clusters known as Pautrier’s microabscesses.
Treatment
Specific regimens
- Hairy cell leukemia
- Chemotherapy with cladribine or pentostatin