| Strategy | Drug Classes / Examples | Primary Target | Goal |
|---|---|---|---|
| Rate Control | β-Blockers (Metoprolol) Non-DHP CCBs (Diltiazem) Digoxin | AV Node | Slow ventricular rate (e.g., < 110 bpm) |
| Rhythm Control | Class Ic (Flecainide) Class III (Amiodarone, Sotalol) | Atrial Myocytes | Restore & maintain Normal Sinus Rhythm |
Class I: Sodium (Na+) Channel Blockers
- Mechanism: Block voltage-gated Na⁺ channels (Phase 0), slowing the rate of depolarization of the action potential. This primarily affects fast-channel tissues (atrial/ventricular myocytes, His-Purkinje system). They exhibit use-dependence, meaning they are more effective at faster heart rates.
- Why it works: By slowing conduction velocity in non-nodal tissue, Class I drugs interrupt reentrant circuits, which are the cause of many tachyarrhythmias.
Class Ia (e.g., Quinidine, Procainamide)
- Effect: Moderate Na⁺ channel blockade + K⁺ channel blockade. Increases AP duration and increases the effective refractory period (ERP). Widens the QRS and prolongs the QT interval on ECG.
- Indications: Both atrial and ventricular arrhythmias, including atrial fibrillation (AF), atrial flutter, and ventricular tachycardia (VT).
- Rationale: The combined effect of slowing conduction and prolonging the refractory period is effective at breaking reentrant rhythms in both the atria and ventricles.
Class Ib (e.g., Lidocaine, Mexiletine)
- Effect: Weak Na⁺ channel blockade. Shortens AP duration. Preferentially acts on ischemic or depolarized tissue.
- Indications: Primarily ventricular arrhythmias (VT, VF), especially in the setting of acute MI. Has minimal effect on atrial tissue.
- Rationale: Ischemic tissue has a more depolarized resting membrane potential, which keeps Na⁺ channels in an inactivated state that Class Ib drugs preferentially bind. This makes them highly effective for arrhythmias originating from ischemic myocardium while sparing healthy tissue.
Class Ic (e.g., Flecainide, Propafenone)
- Effect: Potent Na⁺ channel blockade with slow dissociation. Markedly slows conduction velocity with minimal effect on AP duration. Widens the QRS complex significantly.
- Indications: Supraventricular tachycardias (SVTs) and AF (e.g., “pill-in-the-pocket” strategy).
- Contraindication: CONTRAINDICATED in patients with structural or ischemic heart disease due to increased mortality (proarrhythmic risk).
- Rationale: The profound slowing of conduction is very effective for terminating reentrant SVTs. Its use is limited to structurally normal hearts where this potent effect is less likely to create a new, more dangerous arrhythmia.
Class II: Beta-Blockers (β-Blockers)
- Mechanism: (e.g., Metoprolol, Propranolol) Block β-adrenergic receptors, reducing the effects of catecholamines on the heart. This decreases cAMP levels, which has two key effects:
- Slows the rate of diastolic depolarization (Phase 4) in the SA node, decreasing automaticity.
- Slows conduction through the AV node.
- Effect: Decreases heart rate (negative chronotropy) and contractility (negative inotropy). Prolongs the PR interval on ECG.
- Indications:
- Rate control in AF and atrial flutter.
- Treatment and prevention of SVTs.
- Suppressing catecholamine-induced arrhythmias (e.g., exercise-induced VT).
- Rationale: Excellent for arrhythmias caused by sympathetic overstimulation. By slowing AV conduction, they protect the ventricles from excessively high rates originating in the atria (“rate control”).
Class III: Potassium (K⁺) Channel Blockers
- Mechanism: (e.g., Amiodarone, Sotalol, Dofetilide) Block delayed rectifier K⁺ channels (Phase 3), inhibiting repolarization.
- Effect: Prolongs AP duration and increases the ERP without affecting conduction velocity. This prolongs the QT interval on ECG.
- Indications: Broad-spectrum use for both atrial (AF, atrial flutter) and ventricular arrhythmias (VT, VF). Amiodarone is particularly useful in patients with structural heart disease.
- Rationale: By significantly extending the refractory period, these drugs make the myocardial tissue unexcitable for a longer duration. This prevents reentry, as the reentrant impulse is more likely to encounter tissue that is still refractory and cannot conduct.
Class IV: Non-Dihydropyridine Calcium (Ca2+) Channel Blockers
- Mechanism: (e.g., Verapamil, Diltiazem) Block L-type Ca2+ channels, primarily affecting slow-channel tissues (SA and AV nodes).
- Effect: Similar to β-blockers, they decrease automaticity in the SA node and slow conduction through the AV node. Prolongs the PR interval on ECG.
- Indications:
- Termination of SVT (especially AVNRT).
- Rate control for AF and atrial flutter.
- Rationale: Their primary action on the AV node makes them ideal for treating arrhythmias that involve the AV node as part of a reentrant circuit (AVNRT) or for slowing the ventricular response to rapid atrial rhythms.
Other / Unclassified Antiarrhythmics
- Adenosine
- Mechanism: Activates K⁺ channels in the AV node, causing hyperpolarization and transient AV block.
- Indications: Acute termination of SVT. It is the first-line drug for most forms of stable, narrow-complex SVT.
- Rationale: Its extremely short half-life (~10 seconds) makes it a safe diagnostic and therapeutic agent for acutely “resetting” the AV node to terminate reentrant SVTs.
- Digoxin
- Mechanism: Increases vagal (parasympathetic) tone, which slows conduction through the AV node and decreases heart rate.
- Indications: Rate control in AF, especially in patients with concomitant heart failure.
- Rationale: The combination of slowing AV conduction and providing a positive inotropic effect (improving contractility) is beneficial in patients with both AF and heart failure.
- Magnesium Sulfate (MgS0₄)
- Mechanism: Acts as a Ca2+ channel antagonist and blocks certain K⁺ channels.
- Indications: Torsades de pointes (a specific type of polymorphic VT associated with a long QT interval).
- Rationale: Stabilizes the cardiac membrane and is thought to correct the early afterdepolarizations that trigger Torsades de pointes.
Class I antiarrhythmics
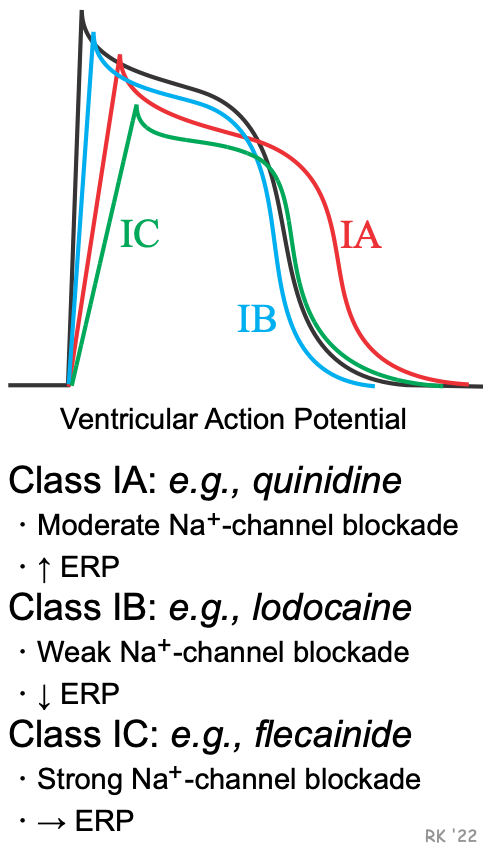 The key here is to separate the effects of sodium channels and potassium channels.
The key here is to separate the effects of sodium channels and potassium channels.
- Sodium channel blockage = slow depolarization + wide QRS + long QT
- Potassium channel blockage = prolonged APD + prolonged ERP. Both of these blocking effects can treat rapid cardiac arrhythmias. Class IA is 1+2, Class IC is only 1 (strongly). However, Class IB is different from the first two as it promotes potassium outflow, thus shortening APD and ERP and increasing ERP:APD ratio
Class III antiarrhythmics
Amiodarone
Tip
Amiodarone has both Class I, II, III & IV actions!
Pharmacodynamics
- Primary mechanism of action: antiarrhythmic effect via blockage of voltage-gated potassium channels → prolonged repolarization of the cardiac action potential
- Secondary mechanism of action: inhibits β-receptors and sodium and calcium channels → decreases conduction through the AV and sinus node
- Special uses: only antiarrhythmic agent with (almost) no negative inotropic effect → use in patients with reduced EF
Other antiarrhythmic drugs
Adenosine
Drawing 2025-06-02 17.09.50.excalidraw
⚠ Switch to EXCALIDRAW VIEW in the MORE OPTIONS menu of this document. ⚠ You can decompress Drawing data with the command palette: ‘Decompress current Excalidraw file’. For more info check in plugin settings under ‘Saving’
Excalidraw Data
Text Elements
Embedded Files
0aaa23e1f56152948c65c0fbb1af755c5f2371eb: Pasted Image 20250602170952_431.png
Link to original
Tip
- Adenosine = Adenine + Ribose
- Major source: ATP/AMP Breakdown, especially during high metabolic activity or stress (e.g., hypoxia, ischemia). ATP → ADP → AMP → Adenosine (via 5’-nucleotidases).
- Normally, the conversion of AMP to adenosine doesn’t frequently occur because it doesn’t produce significant energy. Therefore, an accumulation of adenosine suggests severe energy depletion or cellular distress.
- Adenosine acts as a signaling molecule. It triggers protective responses (e.g., vasodilation to increase blood flow and oxygen supply, slow down heart rate, reduction of cellular metabolic demand, anti-inflammatory effects).
- Mechanism of action: activates Gi protein → inhibition of adenylate cyclase → ↓ cAMP → deactivation of L-type Ca2+ channels and activation of K+ channels → ↓ Ca2+ and ↑ K+ efflux → hyperpolarization → transient AV node block (short-acting, ∼ 15 seconds) → acute termination of supraventricular tachycardia
- Vasodilator
- Coronary autoregulation is a process that maintains myocardial blood flow in settings of decreased coronary perfusion pressure (eg, hemorrhage, sepsis). Within the region of autoregulation (eg, 60-140 mm Hg), changes in coronary blood flow are driven primarily by myocardial oxygen demand. This is accomplished mostly by automated alterations in vascular resistance via the release of locally acting mediators, namely adenosine (released from cardiomyocytes as ATP is broken down for energy) and nitric oxide (synthesized by endothelial cells in response to chemical mediators and mechanical stress).
- When myocardial perfusion pressure decreases, there is decreased oxygen delivery to the myocardium and less ATP is regenerated via oxidative metabolism, resulting in increased levels of adenosine. Myocardial hypoxia also triggers increased synthesis of nitric oxide.
- Indications
- Adverse effects
- Chest pain, flushing, hypotension, bronchospasm
- Sense of impending doom
- AV block, asystole