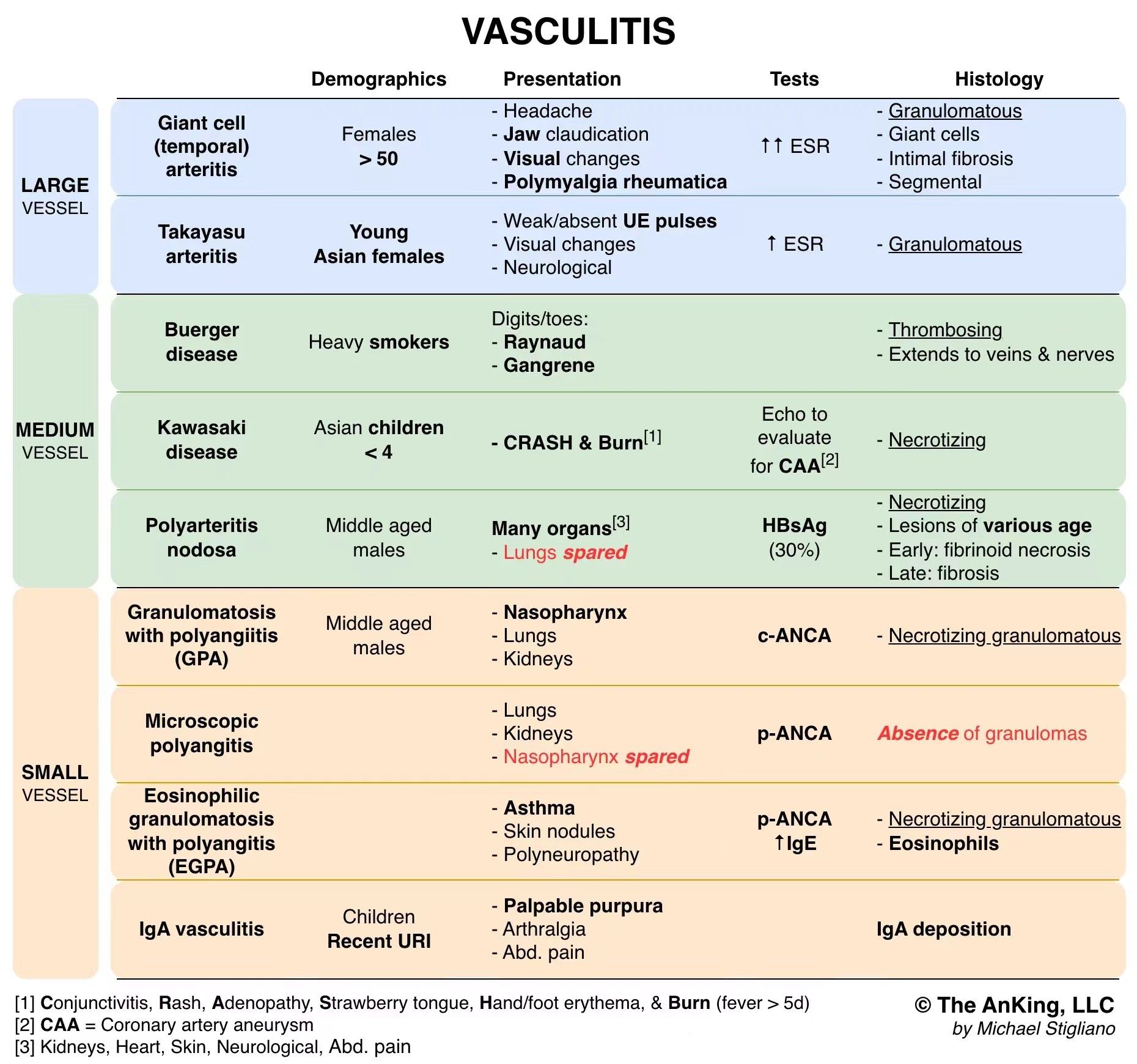
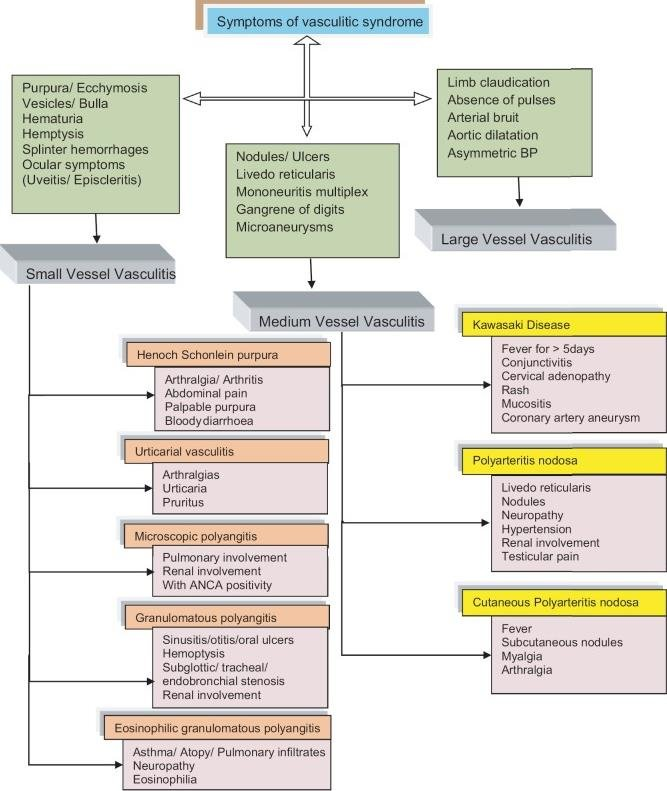
Large-vessel vasculitis
Involves aorta and major branches.
- Giant Cell Arteritis (Temporal arteritis)
- Epidemiology: Elderly females (>50 yo). Associated with Polymyalgia Rheumatica.
- Pathology: Granulomatous inflammation of branches of the carotid artery.
- Clinical Features: Unilateral headache, jaw claudication, potential blindness (ophthalmic artery occlusion).
- Dx: ↑ ESR/CRP. Temporal artery biopsy (segmental lesions require long segment biopsy).
- Tx: High-dose corticosteroids immediately (do not wait for biopsy results to prevent blindness).
- Takayasu Arteritis
- Epidemiology: Asian females <40 yo.
- Pathology: Granulomatous thickening of aortic arch and proximal great vessels.
- Clinical Features: “Pulseless disease” (weak upper extremity pulses), fever, night sweats, skin nodules. Discrepancy in BP between arms.
- Tx: Corticosteroids.
A japanese man get arm cut off.
Medium-vessel vasculitis
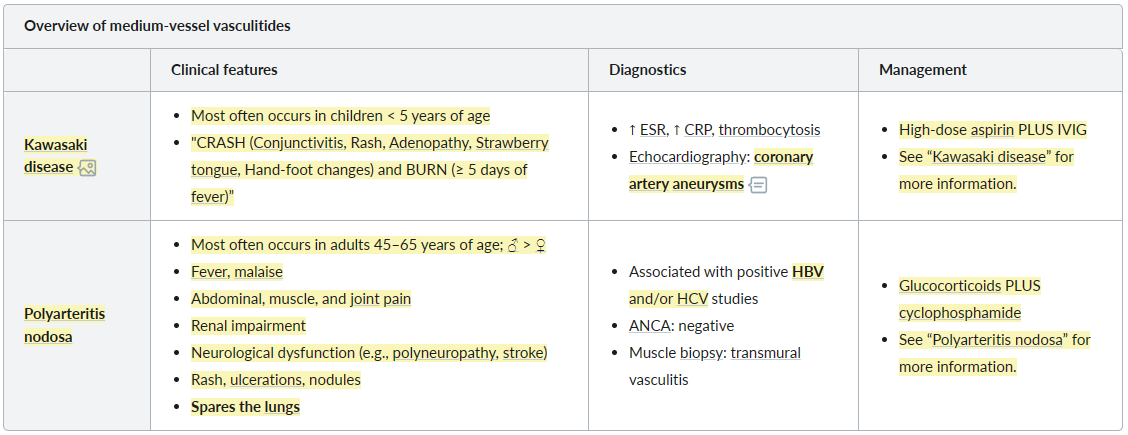 See Polyarteritis nodosa
Also add Thromboangiitis obliterans
See Polyarteritis nodosa
Also add Thromboangiitis obliterans
Clinical features
Link to original
- Migratory superficial thrombophlebitis (recurrent): often seen prior to the onset of limb ischemia
- Tender nodules along the course of the affected vein
- Raynaud phenomenon
- Chronic or acute limb ischemia: may progress from distal to proximal vessels
- Intermittent claudication
- Pain at rest, cool extremities, and/or diminished or absent pulses
- Ulceration and/or gangrene of fingertips and/or toes (digits may autoamputate)
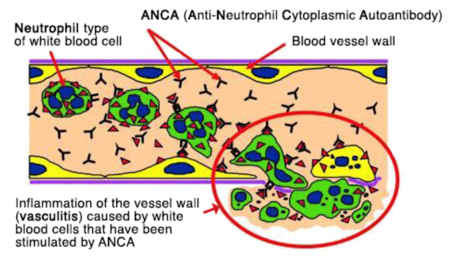
Small-vessel vasculitis
ANCA-associated small-vessel vasculitis t
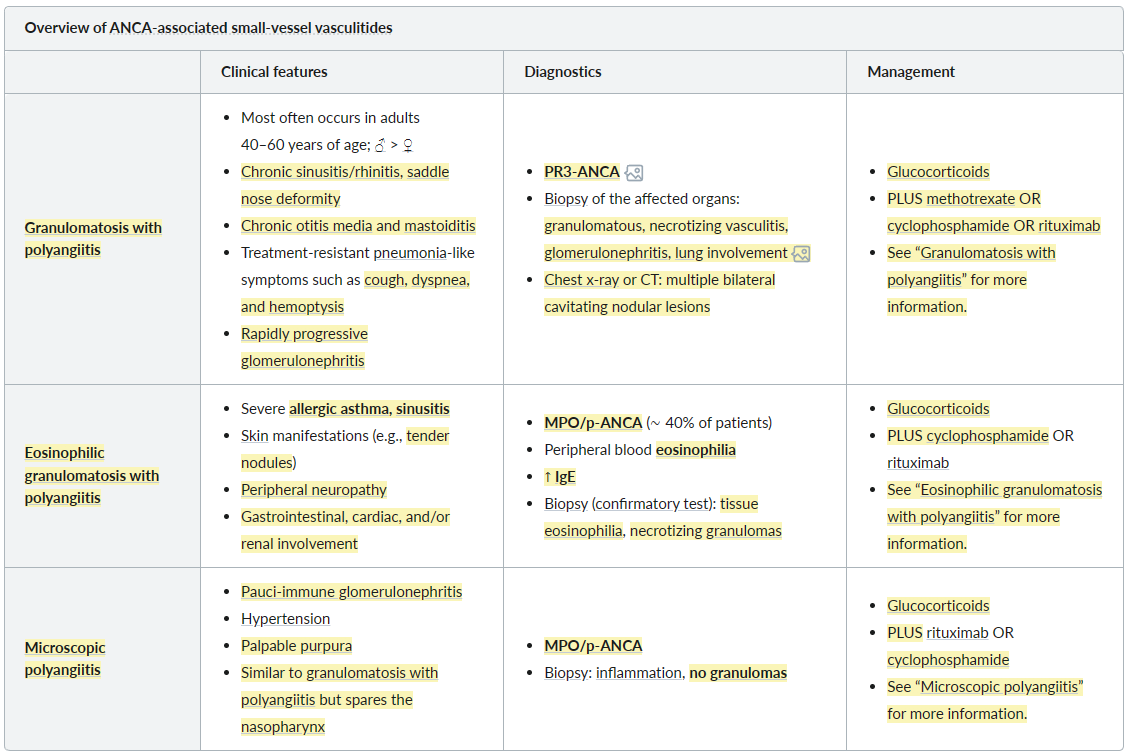 See Granulomatosis with polyangiitis
See Granulomatosis with polyangiitis
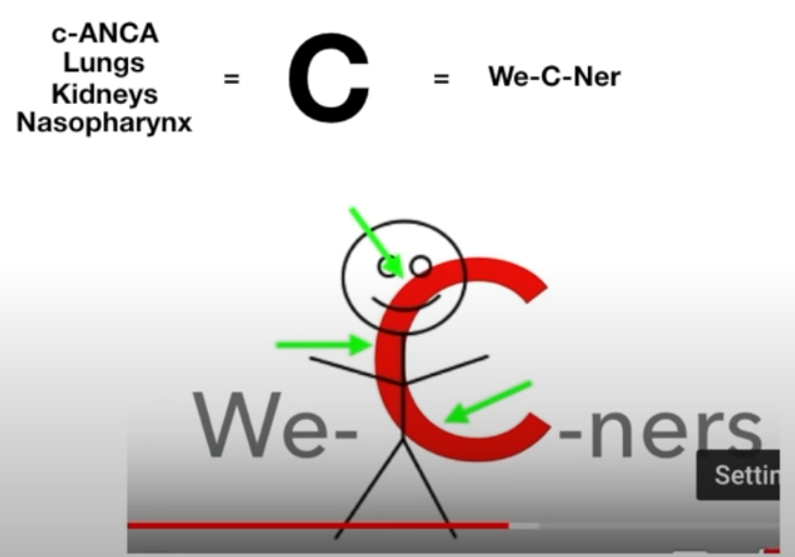
Granulomatosis with polyangiitis (Wegener granulomatosis)
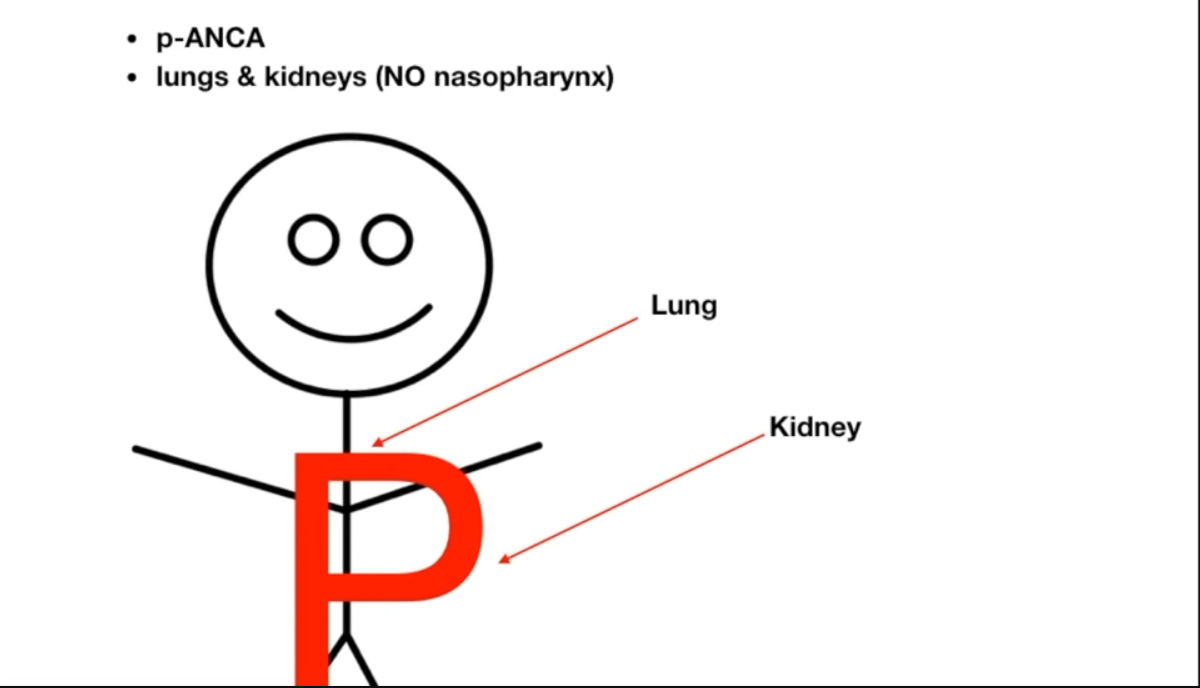
Microscopic polyangiitis
Non-ANCA-associated small-vessel vasculitis
IgA vasculitis, also known as Henoch-Schönlein purpura