Acute tubulointerstitial nephritis
Definition
Acute tubulointerstitial nephritis (ATIN) is an acute inflammation of the renal interstitium and tubules that causes a decline in renal function over a period of days to weeks.
Etiology
Medications (most common)
- Antibiotics: β-lactams, sulfonamides, rifampin, fluoroquinolones
- NSAIDs
- Proton pump inhibitors and H2 blockers
- Loop diuretics and thiazides
- Anticonvulsants: phenytoin, valproate, carbamazepine, phenobarbital
- Other: allopurinol
Pathophysiology
- Immune-mediated tubulointerstitial damage (allergic interstitial nephritis) is the most widely accepted theory.
- Inflammatory infiltrates → tissue edema and tubular cell damage → compromised tubular flow
- Allergic interstitial nephritis: drugs act as haptens → type IV hypersensitivity reaction
- Acute obstruction: crystals (from e.g., uric acid, medications) or proteins (e.g., light chains) obstruct tubules
Clinical features
- Onset is typically 7-10 days after starting the offending drug.
- Classic Triad (present in only 10-15% of pts):
- Fever
- Rash (maculopapular)
- Arthralgias
- Features of Acute Kidney Injury (AKI): Oliguria, ↑ BUN, ↑ Cr.
Diagnostics
- Labs:
- Peripheral eosinophilia.
- ↑ BUN and ↑ serum Cr.
- Urinalysis (UA):
- WBC casts (pathognomonic but not always present).
- Sterile pyuria (WBCs in urine without bacteriuria).
- Eosinophiluria (seen with Wright or Hansel stain; highly specific but not sensitive).
- Mild proteinuria.
- Renal Biopsy (definitive Dx, but not always required):
- Interstitial inflammatory infiltrate (lymphocytes, macrophages, eosinophils).
Tip
Although frequently cited as a diagnostic clue, in clinical practice, urine eosinophils lack sensitivity and specificity for reliably confirming ATIN.
Treatment
Link to original
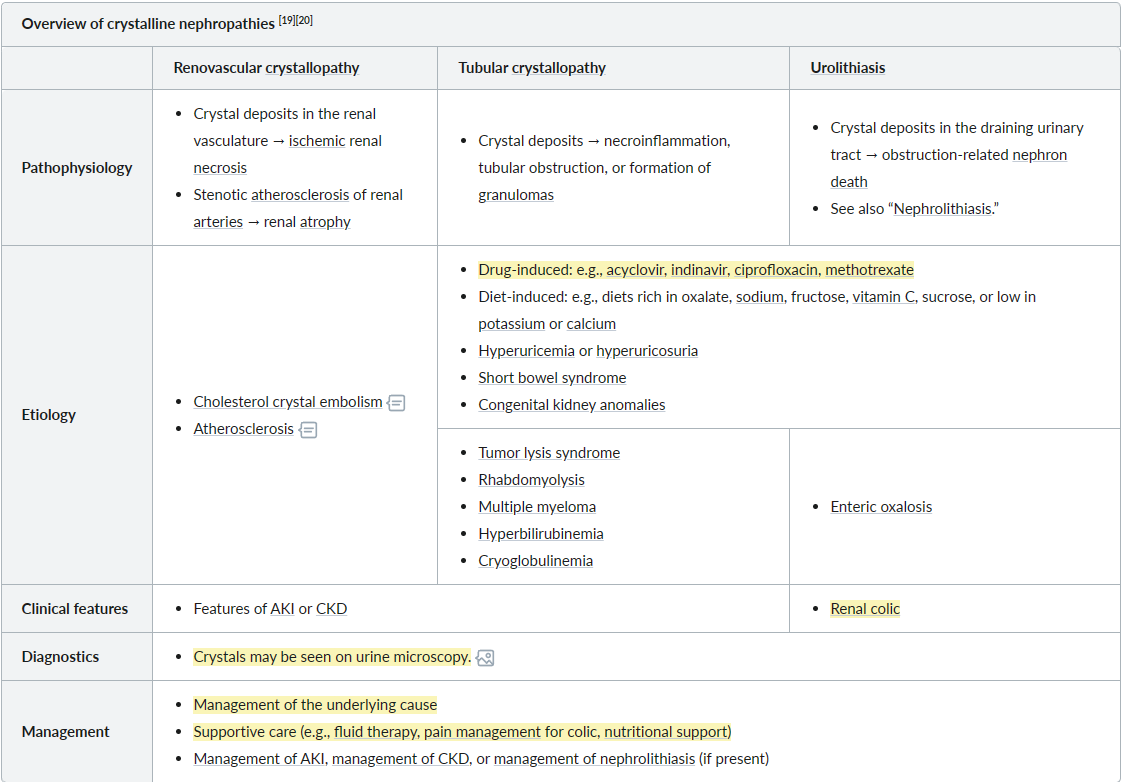
Crystalline nephropathies
Definition: a type of kidney injury that is triggered by crystal deposition and may lead to crystal-induced AKI, crystal-induced CKD, or urolithiasis
Epidemiology
Etiology
Drug-induced: e.g., acyclovir, indinavir, ciprofloxacin, methotrexate
Pathophysiology
Precipitation of minerals (crystallization) → phagocytosis of crystals → activation of the inflammasome → renal damage
Clinical features
Diagnostics
Crystals may be seen on urine microscopy.
Treatment
Link to original
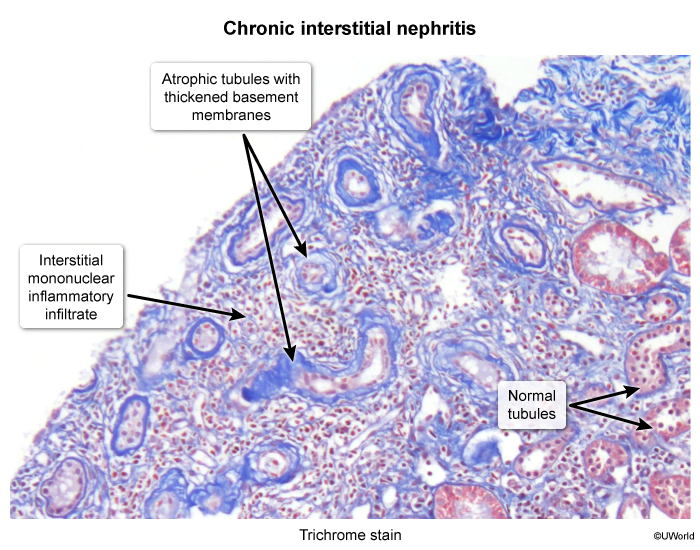
Chronic tubulointerstitial nephritis
Chronic tubulointerstitial nephritis (CTIN) is a condition of chronic inflammation of the renal tubules and interstitium and can progress to end-stage renal disease (ESRD) after months or years.
Pathophysiology
- Analgesic nephropathy (e.g., resulting from NSAIDs use)
- Inhibition of prostacyclin synthesis → vasoconstriction of the medullary blood vessels → papillary ischemia and papillary necrosis
- Associated with an increased risk of urothelial carcinoma; can progress to ESRD
Etiology
- Medications
- Analgesic nephropathy: combination analgesics , NSAIDs, and acetaminophen
Clinical features
- Painless hematuria, pyuria, oliguria, or polyuria
- Colicky flank pain
Diagnostics
Link to original
- Blood tests: ↑ BUN and creatinine, ↓ K+ or ↑ K+; normal anion gap ; anemia of CKD
- Urine chemistries in tubulointerstitial diseases (findings similar to ATIN): sterile pyuria, proteinuria, hematuria, RBC casts, WBC casts
- Renal biopsy: tubulointerstitial fibrosis and tubular atrophy
Renal papillary necrosis
Renal papillary necrosis is ischemic, coagulative necrosis of the renal medullary pyramids and papillae and is a feature of various conditions.
Epidemiology
Etiology
- Often multifactorial
- Sickle cell disease and sickle cell trait
- Acute pyelonephritis
- Obstruction of the urinary tract
- Tuberculosis
- Cirrhosis of the liver
- NSAIDs (due to inhibition of prostaglandin-mediated vasodilation in the vasa recta)
- Diabetes mellitus
Pathophysiology
- Coagulative necrosis of the renal papillae and medullary pyramids due to ischemia. The renal medulla is naturally a low oxygen tension environment, making it vulnerable to ischemic injury.
- Ischemia can result from direct vascular obstruction (e.g., sickle cell), vasoconstriction (e.g., NSAIDs), or inflammation.
Clinical features
- Can be asymptomatic and found incidentally.
- Symptomatic patients may present with:
- Acute flank pain and renal colic (due to obstruction by sloughed papillae).
- Sloughed papillae can obstruct the ureters.
- Gross or microscopic hematuria.
- Fever and chills, especially if a superimposed infection (pyelonephritis) is present.
- Passage of necrotic tissue in the urine.
- Sudden deterioration of kidney function in a patient with a known risk factor (e.g., diabetes) should raise suspicion.
Acute tubular necrosis vs Renal papillary necrosis
- ATN: Oliguria
- Causes: ischemic or toxic
- RPN: Flank pain, hematuria
- Causes: sickle cell disease, NSAIDs
Diagnostics
Treatment
Link to original