Penicillin
Tip
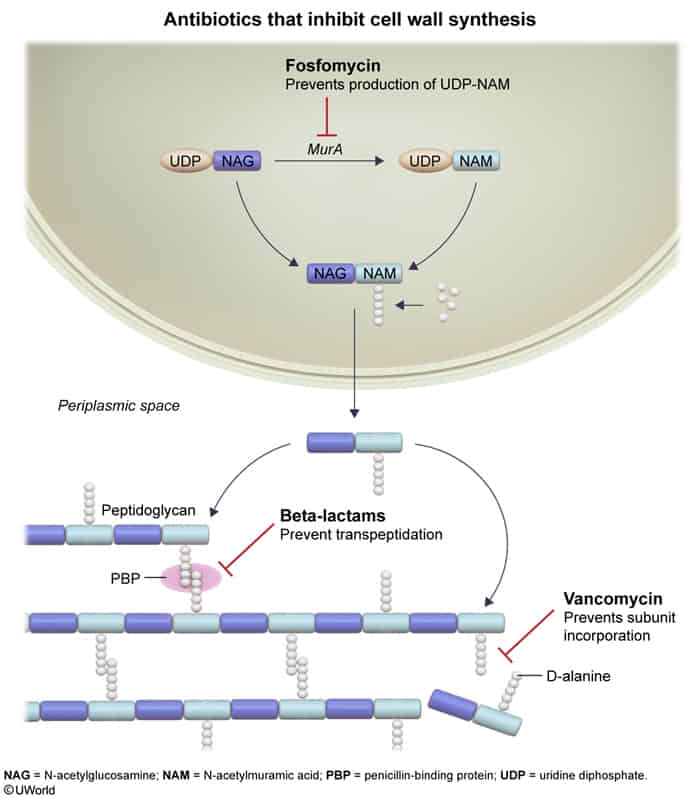
- Penicillin acts as a structural analog of D-Ala-D-Ala. It irreversibly binds to the active site of Penicillin-Binding Proteins (PBPs) (Transpeptidases).
- Vancomycin binds directly to the D-Ala-D-Ala substrate, sterically hindering the transpeptidase enzyme from accessing it.
Types
| Feature | Natural (Pen G/V) | Antistaphylococcal (Nafcillin, Oxacillin) | Aminopenicillins (Ampicillin, Amoxicillin) | Antipseudomonal (Piperacillin) |
|---|---|---|---|---|
| Structural Change | — (parent compound) | + Bulky R-group | + Amino group (polar) | + Extended side chain |
| Pros | — | Bulky group acts like a shield → β-Lactamase resistant | Penetrates Gram(-) porins;↑ Enterococcus/Listeria coverage | Broadest spectrum; Pseudomonas coverage |
| Cons | — | Too big to get into porin → ↓ Gram(-) coverage | Can’t have bulky group → Still β-Lactamase susceptible | Still β-Lactamase susceptible; IV only |
| Spectrum | Narrowest | Narrow | Extended | Broadest |
| Key Targets | Strep, T. pallidum, N. meningitidis | MSSA | + H. flu, E. coli, Listeria, Enterococcus | + Pseudomonas |
| β-Lactamase Resistant? | ❌ | ✅ | ❌ | ❌ |
| + Inhibitor | — | — | Clavulanate, Sulbactam | Tazobactam |
| Route | G: IV/IM; V: PO | IV (Diclox: PO) | IV/PO | IV |
| Classic Use | Syphilis, Strep pharyngitis | MSSA skin/endocarditis | UTI, Otitis, Listeria meningitis | Nosocomial, Febrile neutropenia |
| Pearl | Benzathine = IM depot | Interstitial nephritis | Rash w/ EBV (not allergy) | + Aminoglycoside for synergy |
- MSSA: methicillin-susceptible Staph aureus. Methicillin is the first β-Lactamase resistant penicillin. So MSSA = can be treated by Antistaphylococcal or PCN + β lact inhibitor = can be treated by PCN category antibiotics.
- MRSA: has mecA gene that encodes a modified penicillin-binding protein (PBP) that inhibits the binding of β-lactam antibiotics. = can’t be treated by PCN category antibiotics. Need vancomycin
- Also applies to Coagulase-negative Staphylococci (e.g., S. epidermidis). t
Indications
- Syphilis (Treponema pallidum):
- Drug of Choice: Penicillin G is the only effective treatment for all stages, especially neurosyphilis and syphilis in pregnancy.
- Regimen: Single IM dose of Benzathine Penicillin G for primary/secondary syphilis.
- Streptococcal Pharyngitis (Strep Throat - Group A Strep):
- Drug of Choice: Oral Penicillin V or Amoxicillin for 10 days.
- Key Goal: Prevent acute rheumatic fever. No known resistance of GAS to penicillin.
- Rheumatic Fever Prophylaxis:
- Drug of Choice: Long-acting IM Benzathine Penicillin G (e.g., every 3-4 weeks) for secondary prevention after an initial episode.
- Actinomycosis (Actinomyces israelii):
- Drug of Choice: High-dose IV Penicillin G for an extended period, followed by oral therapy.
- Buzzwords: “Sulfur granules,” jaw/cervicofacial abscess.
- Leptospirosis (Leptospira spp.):
- Drug of Choice: IV Penicillin G is used for severe disease.
- Presentation: Flu-like illness, conjunctival suffusion, myalgias, often with animal/water exposure.
- Meningococcal Disease (Neisseria meningitidis):
- Drug of Choice: Penicillin G is effective if the isolate is susceptible (though ceftriaxone is often used empirically first).
Drug Interactions
- Probenecid
- Mechanism: Competitively inhibits renal tubular secretion of penicillins in the proximal tubule.
- Effect: ↓ renal clearance of PCN → ↑ serum concentration and prolongs the half-life.
- Don’t mix with Tazobactam (β-lactamase inhibitor) t
- Historical Use: To “boost” PCN levels, especially in the treatment of neurosyphilis or gonorrhea, to ensure adequate drug exposure.
- Methotrexate (MTX)
- Mechanism: PCNs compete with MTX for renal tubular secretion.
- Effect: ↓ renal clearance of MTX.
- Clinical Consequence: Can lead to methotrexate toxicity (myelosuppression, mucositis, liver/kidney injury).
- Warfarin
- Mechanism: Broad-spectrum penicillins can eliminate gut flora that synthesize vitamin K.
- Effect: May potentiate the anticoagulant effect of warfarin, leading to an ↑ INR and ↑ bleeding risk. This is a general effect of many broad-spectrum antibiotics.
Cephalosporins
Mnemonic
Cephalosporins are LAME: 1st–4th generation cephalosporins do not act against
- Listeria
- Atypical organisms (e.g., Chlamydia, Mycoplasma)
- No cell wall
- MRSA
- Enterococci (with the exception of ceftaroline, which does act against MRSA).
Nitrofurans
- Examples: nitrofurantoin
- Mechanism of action: reduced by bacterial nitroreductases to reactive metabolites → bind to bacterial ribosomes → impaired metabolism, impaired synthesis of protein, DNA, and RNA → cell death (bactericidal effect)
- Treatment and prophylaxis of acute uncomplicated UTIs (e.g., urethritis, cystitis)
Fluoroquinolone
- Adverse Effects (High-Yield)
- Musculoskeletal: Tendonitis and Achilles tendon rupture (BLACK BOX WARNING). Risk is ↑ in elderly, pts on steroids, and transplant recipients.
- Articular Cartilage Damage: Contraindicated in pregnant women and children due to potential for arthropathy (observed in animal studies).
- Cardiovascular: QT interval prolongation, which can lead to Torsades de pointes.
- CNS: Confusion, headache, dizziness, seizures (rare).
- GI: Nausea, vomiting, diarrhea (may ↑ risk for C. difficile infection).
- Dermatologic: Photosensitivity.
- Drug Interactions
- Ciprofloxacin inhibits Cytochrome P450.
- Chelation with divalent/trivalent cations (Ca, Mg, Fe) → avoid milk/antacids.
Metronidazole
- Mechanism of Action
- A prodrug that is activated in anaerobic organisms and certain protozoa.
- Reductive activation by proteins like ferredoxin creates cytotoxic free radicals that bind to and disrupt DNA structure, causing cell death.
- Key Uses:
- Trichomoniasis (vaginitis)
- Bacterial Vaginosis (Gardnerella)
- Amebiasis, Giardiasis
- C. difficile colitis
- Toxicity/Side Effects:
- Disulfiram-like reaction with alcohol. t
- Metallic taste.
- Neurotoxicity (high dose/prolonged use).
- Major Interaction:
- Increases warfarin effect (↑ INR).
Vancomycin
- Class: Glycopeptide antibiotic.
- Mechanism: Inhibits bacterial cell wall synthesis by directly binding to D-Ala-D-Ala precursors. t
- Spectrum: Gram-positive organisms ONLY.
- High-Yield Uses:
- IV: MRSA infections (bacteremia, pneumonia, endocarditis).
- PO: Clostridioides difficile colitis (not absorbed).
- Key Adverse Effects:
- Red Man Syndrome: Histamine-mediated flushing (slow infusion rate to prevent). NOT a true allergy.
- Nephrotoxicity: Requires therapeutic drug monitoring (trough levels).
- Ototoxicity: Rare, increased risk with other ototoxic agents.
- Mechanism of Resistance:
- Modification of the binding site from D-Ala-D-Ala to D-Ala-D-Lac. Classic in VRE.
TMP-SMX
- Adverse Effects:
- Hyperkalemia (TMP blocks Na⁺ channels in the collecting duct, similar to amiloride). t
- Megaloblastic anemia (Rescue: Leucovorin).
- G6PD Hemolysis (Bite cells).
- SJS/TEN, Photosensitivity.
- Kernicterus (Neonates).
- Artificial ↑ Creatinine.
Drug resistance
Mechanisms
| Type of resistance | Example mechanisms | Example antibiotics affected |
|---|---|---|
| Increased drug efflux pump | • New membrane transport system | • Tetracyclines, fluoroquinolones |
| Drug-inactivating enzyme | • Beta-lactamase • Acetyltransferase | • Penicillins, cephalosporins • Aminoglycosides |
| Decreased drug uptake | • Mutated porin protein | • Penicillins, fluoroquinolones |
| Modified drug target | • Altered penicillin-binding protein • Altered ribosomal protein • Altered DNA gyrase | • Penicillins • Aminoglycosides, macrolides • Fluoroquinolones |
Examples
1. MRSA (Methicillin-Resistant Staphylococcus aureus)
- Clues: Purulent skin/soft tissue infections (SSTIs) often looking like “spider bites” (CA-MRSA); hospital-acquired pneumonia, post-op infections, line infections (HA-MRSA). Post-influenza pneumonia.
- Mechanism: mecA gene (altered PBP2a).
- Tx:
- SSTI (CA): TMP-SMX, Doxycycline, Clindamycin (after I&D).
- Severe/Hospital (HA): Vancomycin, Linezolid, Daptomycin.
2. VRE (Vancomycin-Resistant Enterococci)
- Clues: UTI, bacteremia in hospitalized patients with prolonged antibiotic use (especially vancomycin/cephalosporins) or indwelling catheters.
- Mechanism: D-Ala-D-Ala to D-Ala-D-Lac/Ser.
- Tx: Linezolid, Daptomycin. (Nitrofurantoin/Fosfomycin for cystitis if susceptible).
3. Extended-Spectrum Beta-Lactamase (ESBL)-Producing Enterobacterales (E. coli, Klebsiella)
- Clues: Recurrent UTIs despite cephalosporins; hospital/LTCF-acquired infections (UTI, intra-abdominal).
- Mechanism: Beta-lactamases hydrolyzing most penicillins & cephalosporins.
- Tx: Carbapenems (Imipenem, Meropenem). (Fosfomycin/Nitrofurantoin for cystitis if susceptible).
4. CRE (Carbapenem-Resistant Enterobacterales - e.g., Klebsiella pneumoniae carbapenemase/KPC)
- Clues: Critically ill ICU patients; multiple prior antibiotics (including carbapenems); invasive devices. High mortality.
- Mechanism: Carbapenemase enzymes.
- Tx: Very limited; often combination therapy with newer agents (e.g., Ceftazidime-avibactam, Meropenem-vaborbactam) or Colistin/Tigecycline.
5. Drug-Resistant Streptococcus pneumoniae
- Clues: CAP, meningitis, otitis media failing first-line beta-lactams. Risk factors: age extremes, daycare, recent antibiotics.
- Mechanism: Altered PBPs (penicillin resistance); ribosomal methylation/efflux (macrolide resistance).
- Tx:
- CAP (non-meningeal): Respiratory Fluoroquinolones (Levofloxacin, Moxifloxacin), Vancomycin (if severe/highly resistant). Ceftriaxone (if lower-level penicillin resistance).
- Meningitis: Vancomycin + 3rd gen Cephalosporin (e.g., Ceftriaxone).
6. MDR-TB & XDR-TB (Multidrug/Extensively Drug-Resistant Tuberculosis)
- Clues: Prior TB treatment failure; from high-prevalence area; HIV co-infection; persistent TB symptoms despite standard therapy.
- MDR: Resistant to Isoniazid (INH) + Rifampin (RIF).
- XDR: MDR + resistance to a fluoroquinolone AND ≥1 injectable second-line drug.
- Mechanism: Chromosomal mutations (e.g., katG, rpoB).
- Tx: Complex, prolonged multi-drug regimens with second-line drugs (e.g., Bedaquiline, Linezolid, Fluoroquinolones) based on DST. Expert consultation mandatory.
7. Multidrug-Resistant Pseudomonas aeruginosa
- Mechanism: High intrinsic and acquired resistance using multiple strategies simultaneously, including efflux pumps, mutations in porin channels (reducing drug entry), and production of various β-lactamases.