Overview
Mnemonic
- Ectoderm: The outermost layer → develops into structures that interact with the external world (skin, nervous system)
- Mesoderm: The middle layer → develops into supportive structures (muscles, bones, blood-related (heart, vessels, spleen, kidney))
- Endoderm: The innermost layer → develops into internal organs and linings (digestive tract, lungs)
- Ectoderm
- Surface ectoderm
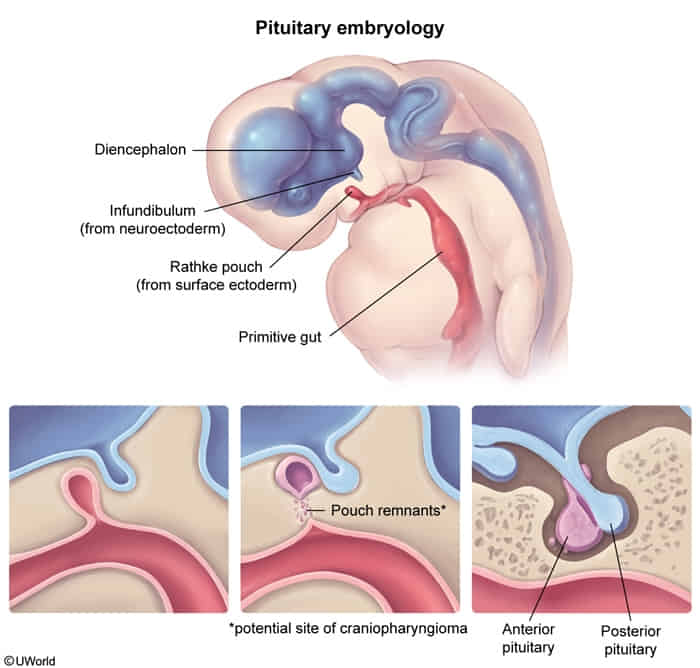
- Anterior pituitary (Rathke pouch)
- Anterior pituitary gland (adenohypophysis): develops from oral ectoderm (Rathke pouch)
- Posterior pituitary gland (neurohypophysis): develops from neural ectoderm
- Lens & cornea
- Inner ear sensory organs, olfactory epithelium
- Nasal & oral epithelial linings, salivary glands
- Epidermis, sweat & mammary glands
- Anterior pituitary (Rathke pouch)
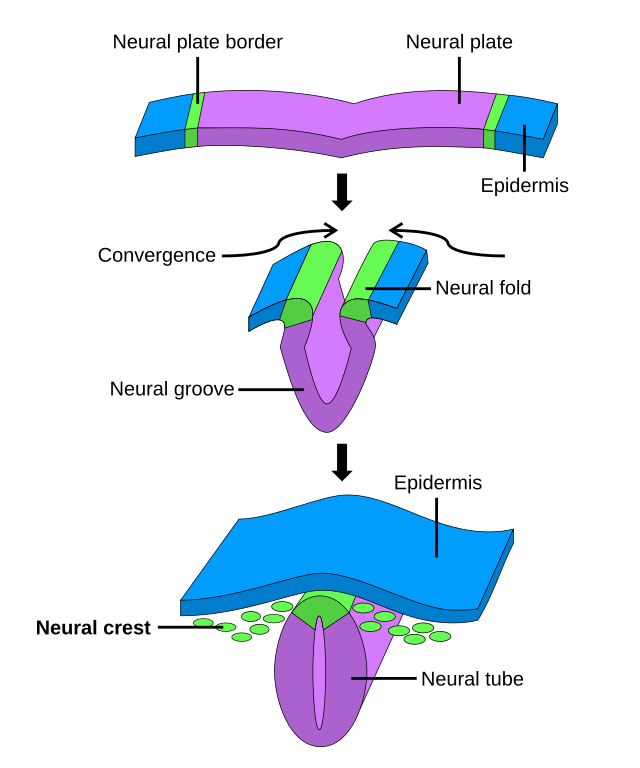
- Neural tube
- Brain & spinal cord
- Posterior pituitary, pineal gland
- Retina
- Neural crest
- Neural ganglia, adrenal medulla
- Schwann cells; pia & arachnoid mater
- Aorticopulmonary septum & endocardial cushions
- Branchial arches (bones & cartilage)
- Skull bones
- Melanocytes
- Surface ectoderm
| Feature | Neural Tube | Neural Crest |
|---|---|---|
| Origin | Forms from the folding of the central ectodermal neural plate. | Arises from migratory cells at the lateral edges of the neural plate. |
| Core System | Central Nervous System (CNS) | Peripheral Nervous System (PNS) + various non-neuronal tissues. |
| Key Derivatives | Brain & Spinal Cord CNS Neurons (motor, interneurons) Oligodendrocytes, Astrocytes, Ependymal cells Posterior Pituitary | PNS (Schwann cells, all ganglia) Melanocytes Adrenal Medulla Craniofacial bones Aorticopulmonary septum |
| Associated Pathologies | Neural Tube Defects (NTDs) - Anencephaly - Spina Bifida (Occulta, Meningocele, Myelomeningocele) | Neurocristopathies - Hirschsprung Disease - Neurofibromatosis - Pheochromocytoma - DiGeorge Syndrome - Melanoma |
| Key Marker | Folate deficiency is a major risk factor for defects. | Defects are often related to abnormal cell migration. |
- Mesoderm
- Muscles (skeletal, cardiac & smooth)
- Connective tissue, bone & cartilage
- Serosal linings (eg, peritoneum)
- Cardiovascular & lymphatic system
- Spleen & hemopoietic cells
- Kidney & ureters, internal genitalia
- Adrenal cortex
- Endoderm
- Gastrointestinal tract, liver, pancreas
- Lungs
- Thymus, parathyroids, thyroid follicular cells
- Middle ear epithelium
- Bladder & urethra
- Parafollicular (C) cells*
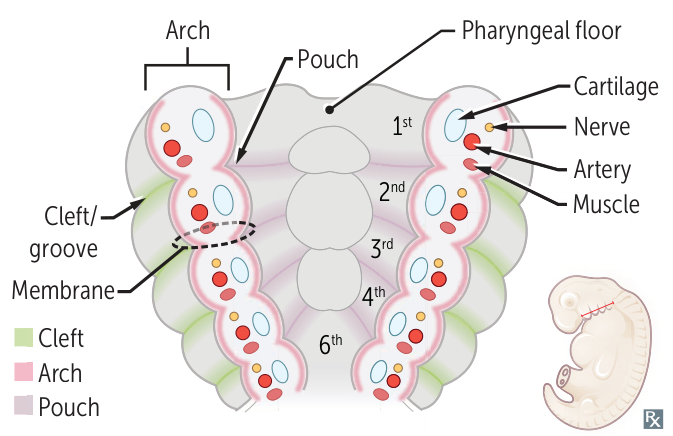
Pharyngeal apparatus
- Pharyngeal clefts—derived from ectoderm. Also called pharyngeal grooves.
- Just external ear canal
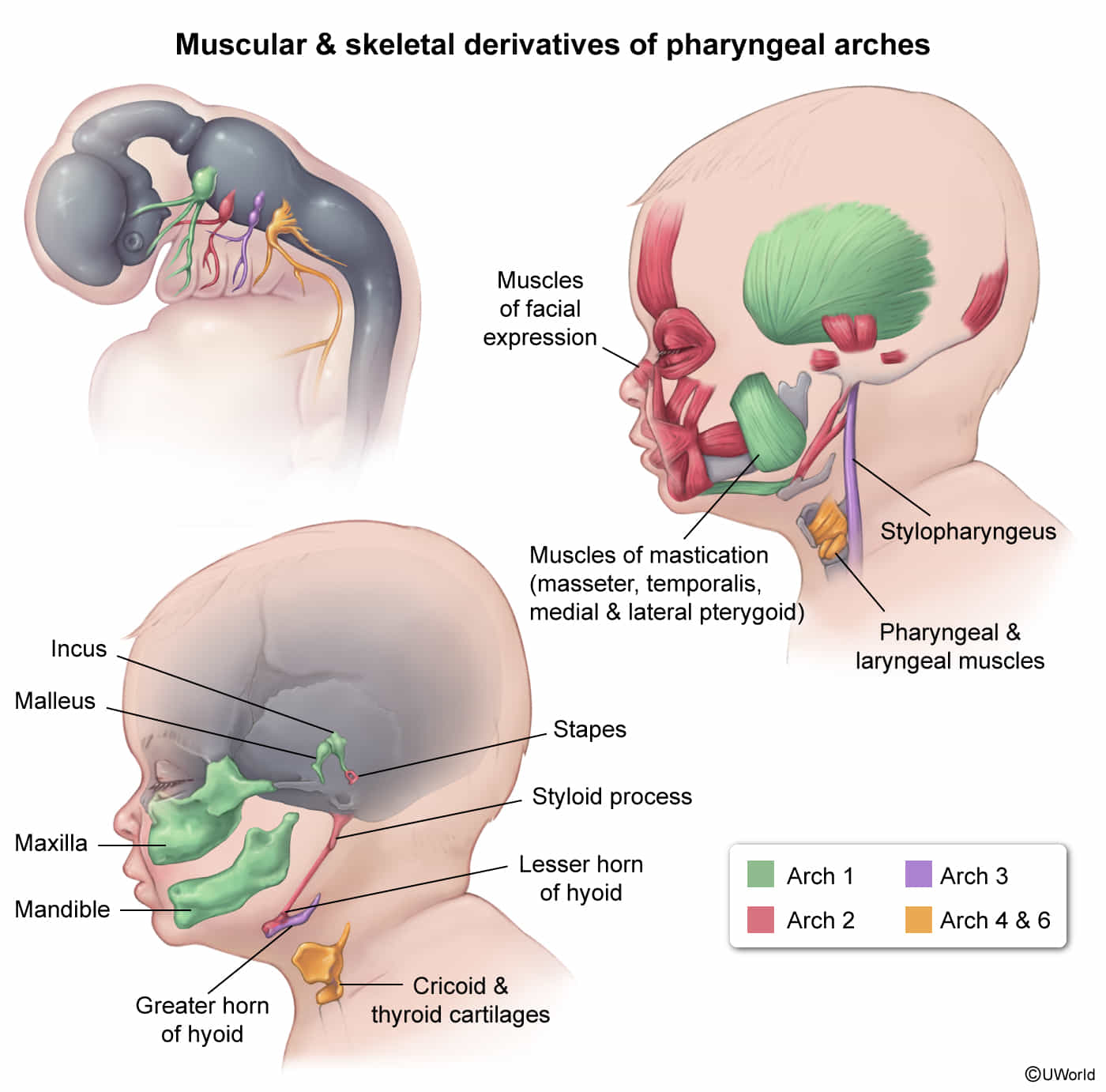
- Pharyngeal arches—derived from mesoderm (muscles, arteries) and neural crest (bones, cartilage).
- Connective tissue
- Cartilage
- Muscle
- Bones
- Nerves
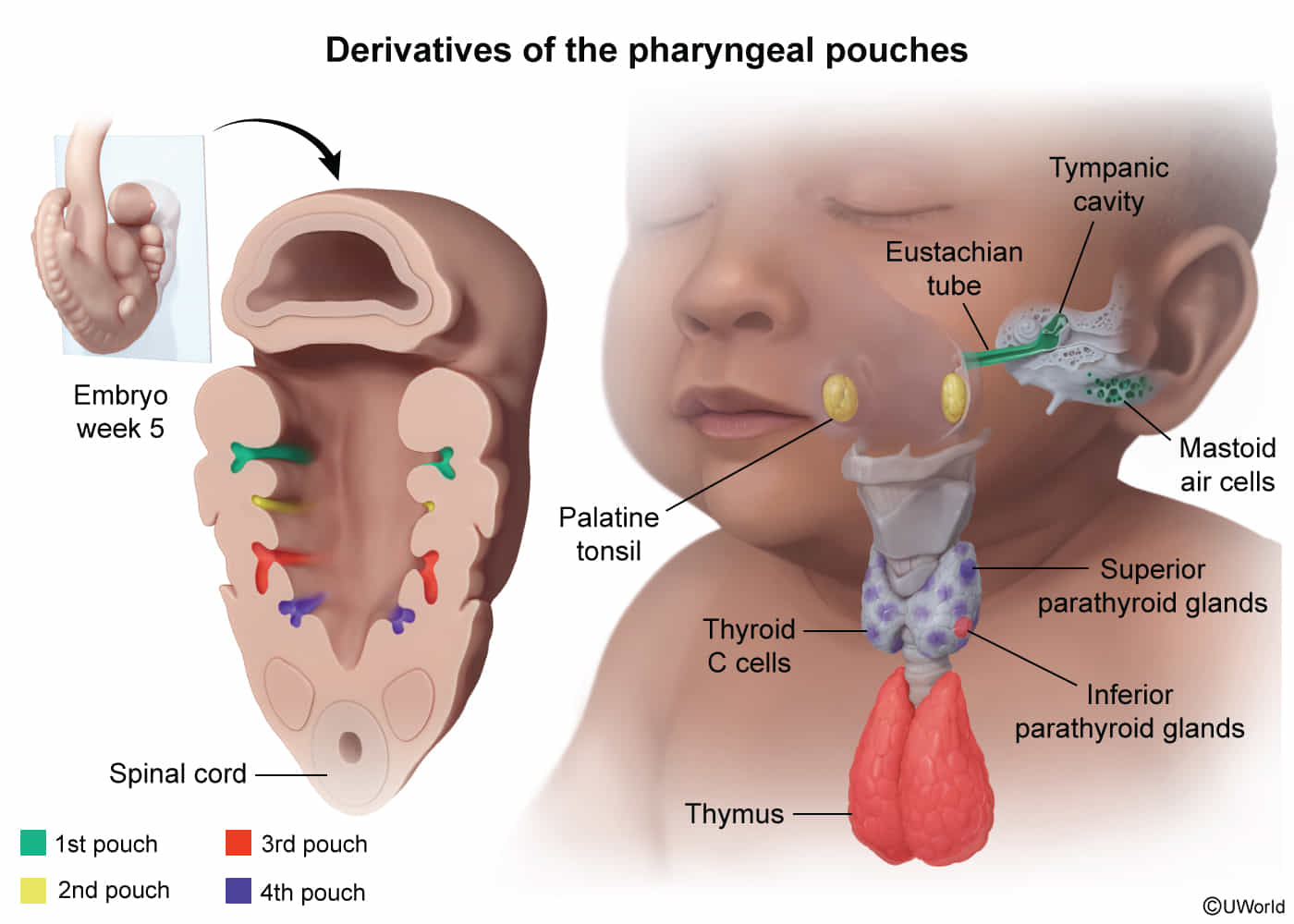
- Pharyngeal pouches—derived from endoderm.
- Epithelium
- Glands
Mnemonic
CAP covers outside to inside:
- Clefts = ectoderm
- Arches = mesoderm + neural crest
- Pouches = endoderm
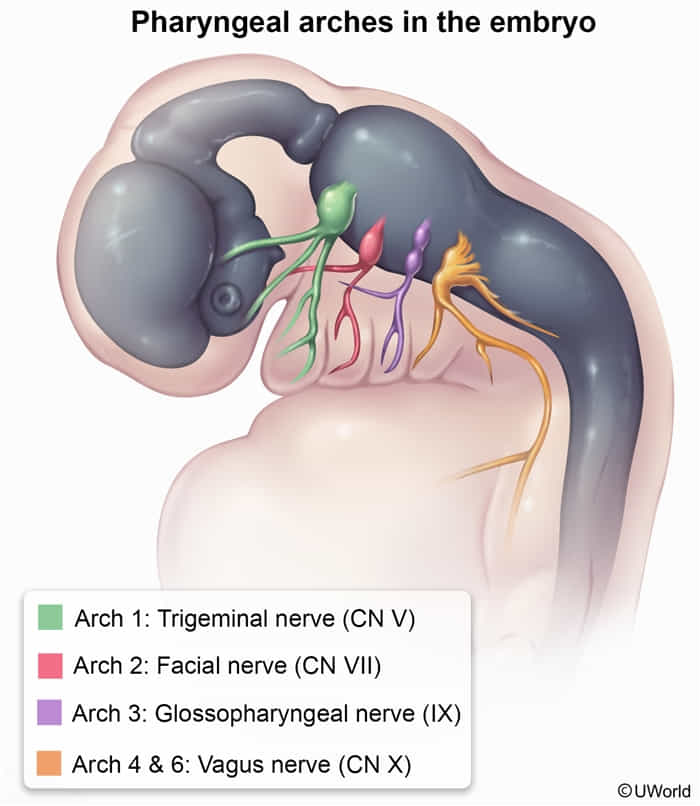
Pharyngeal arch derivatives
When at the restaurant of the golden arches, children tend to first chew (1), then smile (2), then swallow stylishly (3) or simply swallow (4), and then speak (6).
| ARCH | NERVES | MUSCLES | CARTILAGE |
|---|---|---|---|
| 1st pharyngeal arch | CN V3 chew | Muscles of mastication (temporalis, masseter, lateral and medial pterygoids), mylohyoid, anterior belly of digastric, tensor tympani, anterior 2/3 of tongue, tensor veli palatini | Maxillary process → maxilla, zygomatic bone Mandibular process → Meckel cartilage → mandible, malleus and incus, sphenomandibular ligament |
| 2nd pharyngeal arch | CN VII (seven) — smile | Muscles of facial expression, stapedius, stylohyoid, platysma, posterior belly of digastric | Reichert cartilage → stapes, styloid process, lesser horn of hyoid, stylohyoid ligament |
| 3rd pharyngeal arch | CN IX — swallow stylishly | Stylopharyngeus | Greater horn of hyoid |
| 4th and 6th pharyngeal arches | 4th arch: CN X (superior laryngeal branch) simply swallow 6th arch: CN X (recurrent laryngeal branch) speak | 4th arch: most pharyngeal constrictors; cricothyroid, levator veli palatini 6th arch: all intrinsic muscles of larynx except cricothyroid | Arytenoids, Cricoid, Corniculate, Cuneiform, Thyroid cartilage (used to sing and ACCCT) |
Pharyngeal pouches derivatives
Ear, tonsils, bottom-to-top: 1 (ear), 2 (tonsils), 3 dorsal (bottom = inferior parathyroids), 3 ventral (to = thymus), 4 (top = superior parathyroids). t
| POUCH | DERIVATIVES | NOTES |
|---|---|---|
| 1st pharyngeal pouch | Middle ear cavity, eustachian tube, mastoid air cells | 1st pouch contributes to endoderm-lined structures of ear |
| 2nd pharyngeal pouch | Epithelial lining of palatine tonsil | |
| 3rd pharyngeal pouch | Dorsal wings inferior parathyroids Ventral wings thymus | Third pouch contributes to thymus and both inferior parathyroids Structures from 3rd pouch end up below those from 4th pouch |
| 4th pharyngeal pouch | Dorsal wings superior parathyroids Ventral wings ultimopharyngeal body parafollicular (C) cells of thyroid | 4th pharyngeal pouch forms para“4”llicular cells Developmental anomalies in 3rd and 4th pharyngeal pouch are present in DiGeorge syndrome |
 5、7、9、10为混杂
5、7、9、10为混杂
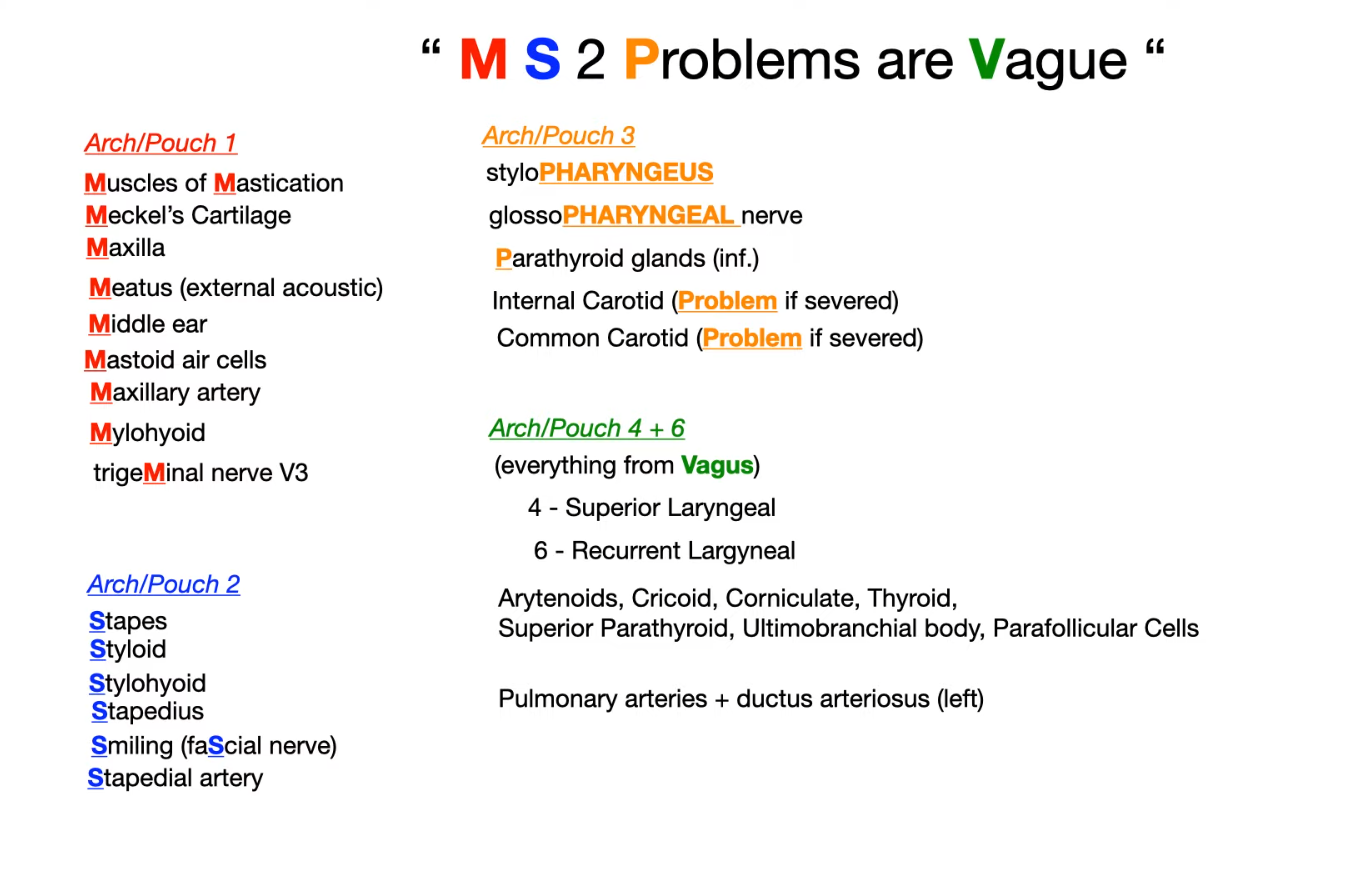 (Medical school 2 problems)
(Medical school 2 problems)
Key Clinical Correlations
- Treacher Collins Syndrome: A first arch neurocristopathy leading to mandibular, maxillary, and zygomatic bone hypoplasia.
- Branchial Cleft Cyst: Results from the failure of the 2nd, 3rd, or 4th cleft (cervical sinus) to obliterate. Presents as a lateral neck mass anterior to the sternocleidomastoid muscle.
- DiGeorge Syndrome (22q11 deletion): Defective development of the 3rd and 4th pouches. Leads to thymic aplasia (T-cell deficiency), hypoparathyroidism (hypocalcemia), and cardiac/facial abnormalities.
- Thyroglossal Duct Cyst: A midline neck mass that moves with swallowing, resulting from the persistence of the thyroglossal duct, which is separate from the pharyngeal apparatus development.