Microscopic anatomy
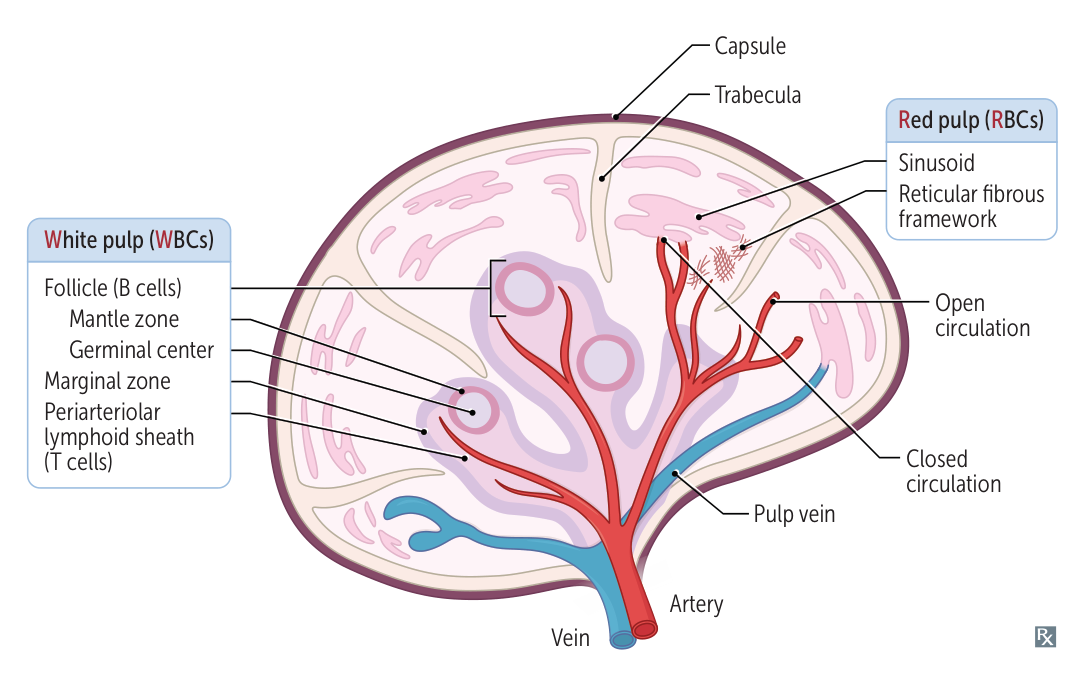
Red pulp
Red pulp is composed of splenic cords and sinuses (sinusoids).
- Splenic cords: a reticular meshwork filled with blood (open circulation system) that filters the blood from damaged erythrocytes
- Spleen sinusoids: long vessels with a fenestrated ring-like (“barrel hoop”) basement membrane that prevent old or malformed RBCs/platelets from reentering venous circulation
- Open circulation: Blood empties from sheathed capillaries into the splenic cords and then enters the sinusoids through slits in the vessel wall.
- Closed circulation: Blood empties from sheathed capillaries of the red pulp directly into the sinusoids.

- Macrophages: found in the cords and around the sinusoids
- Phagocytosis of damaged RBCs/platelets that do not reenter circulation
- Capture of viruses and opsonized pathogens that enter the red pulp
- Blood flow: splenic artery → arterioles → red pulp (cords → sinusoids) → venules → splenic vein → portal circulation
White pulp
- Periarteriolar lymphatic sheath
- Surrounds the arterioles
- Dense lymphoid tissue containing T lymphocytes
- Splenic follicles
- Main component of white pulp
- Close to periarteriolar lymphatic sheath
- Contain B lymphocytes
- Splenic marginal zone
- Located between the red pulp and white pulp
- Contains antigen-presenting cells (APCs): macrophages and specialized B cells (marginal zone B cells)
Spleen Manifestations in Disease
The spleen’s primary roles are filtering blood and mounting immune responses. Its dysfunction or enlargement is a key sign of various systemic diseases. Spleen manifestations can be broadly categorized into Splenomegaly (enlargement) and Hyposplenism/Asplenia (decreased or absent function).
Splenomegaly (Enlarged Spleen)
Enlargement occurs via three main mechanisms:
- Congestion: Due to backup of blood.
- Infiltration: By abnormal cells (e.g., cancer, lipid-laden macrophages).
- Work Hypertrophy/Hyperplasia: Increased filtering or immune activity.
Clinical Presentation:
- Often asymptomatic; may present with early satiety, abdominal fullness, or LUQ pain.
- Palpable spleen below the left costal margin (a normal spleen is usually not palpable).
Key Causes & Associations:
- Congestive Splenomegaly:
- Portal Hypertension: Most common cause. Cirrhosis, portal/splenic vein thrombosis.
- Congestive Heart Failure (CHF): Right-sided heart failure leads to systemic venous congestion.
- Hematologic Disorders:
- Hemolytic Anemias: Hereditary spherocytosis, Sickle Cell Disease (in children, before autosplenectomy), Thalassemia major, Autoimmune Hemolytic Anemia. The spleen enlarges as it removes defective RBCs.
- Myeloproliferative Neoplasms: CML, polycythemia vera, essential thrombocythemia, myelofibrosis. Often cause massive splenomegaly (>1000g or >8 cm below costal margin).
- Leukemias/Lymphomas: Hairy cell leukemia (massive), CLL, Hodgkin & Non-Hodgkin lymphomas.
- Infections:
- Infectious Mononucleosis (EBV): Splenomegaly is common; risk of spontaneous rupture with minor trauma.
- Malaria & Leishmaniasis (Kala-azar): Classic causes of massive splenomegaly.
- Bacterial: Endocarditis, tuberculosis.
- Infiltrative/Storage Diseases:
- Gaucher Disease: Classic lysosomal storage disease causing massive splenomegaly due to accumulation of glucocerebrosides in macrophages (“Gaucher cells”).
- Niemann-Pick Disease: Accumulation of sphingomyelin.
- Sarcoidosis & Amyloidosis: Infiltration by granulomas or amyloid protein, respectively.
Hyposplenism & Asplenia
This refers to decreased or absent splenic function, leading to impaired blood filtering and immune response.
Pathophysiology/Etiology:
- Splenectomy: Surgical removal (e.g., for trauma, ITP, hereditary spherocytosis).
- Autosplenectomy: Repetitive infarction and fibrosis, classically seen in Sickle Cell Disease in adults.
- Congenital Asplenia: Rare developmental failure.
- Functional Hyposplenism: Spleen is present but dysfunctional (e.g., celiac disease, SLE, inflammatory bowel disease).
Diagnosis (Hallmark Peripheral Smear Findings):
- Howell-Jolly bodies: Basophilic nuclear remnants in RBCs (normally removed by spleen). Their presence is a key sign of hyposplenism.
- Target cells (Codocytes): Due to altered RBC membrane.
- Thrombocytosis: Loss of splenic sequestration of platelets.
- Acanthocytes (Spur cells): Spiky RBCs.
Complications & Management:
- Overwhelming Post-Splenectomy Infection (OPSI): High risk of fulminant sepsis from encapsulated organisms due to loss of opsonizing IgM production and phagocytosis. t
- Key Pathogens: Streptococcus pneumoniae (most common), Haemophilus influenzae type b, Neisseria meningitidis.
- Mnemonic: SHiN
- Prevention:
- Vaccinations: Administer vaccines against pneumococcus, meningococcus, and H. influenzae type b, ideally before elective splenectomy or as soon as possible after.
- Prophylactic Antibiotics: Often prescribed, especially for children and the immunocompromised (e.g., penicillin).
- Patient Education: Advise patients to seek immediate medical care for fevers.
| Disease | Spleen Finding | Mechanism |
|---|---|---|
| Sickle Cell Disease | Splenomegaly (in children) → Autosplenectomy (in adults) | Vaso-occlusion from sickled RBCs causes initial splenic sequestration crisis, followed by recurrent infarctions leading to a shrunken, fibrotic spleen. |
| Hereditary Spherocytosis | Splenomegaly | ”Work hypertrophy” from clearing spherocytic RBCs. Splenectomy is curative. |
| Infectious Mononucleosis (EBV) | Splenomegaly | Lymphoid hyperplasia in response to viral infection. High risk of rupture. |
| Portal Hypertension | Congestive Splenomegaly | Increased pressure in the splenic vein obstructs outflow. |
| Myelofibrosis | Massive Splenomegaly | Extramedullary hematopoiesis (blood cell production shifts to spleen as bone marrow fails). |
| Hairy Cell Leukemia | Massive Splenomegaly | Infiltration of the red pulp by neoplastic B-cells. |
| ITP | Normal Spleen Size or Mild Splenomegaly | Spleen is the site of platelet destruction, but does not typically cause significant enlargement. |