- Pathophysiology/Etiology: The final common pathway is a transient drop in cerebral blood flow. The main causes are broadly categorized into three groups:
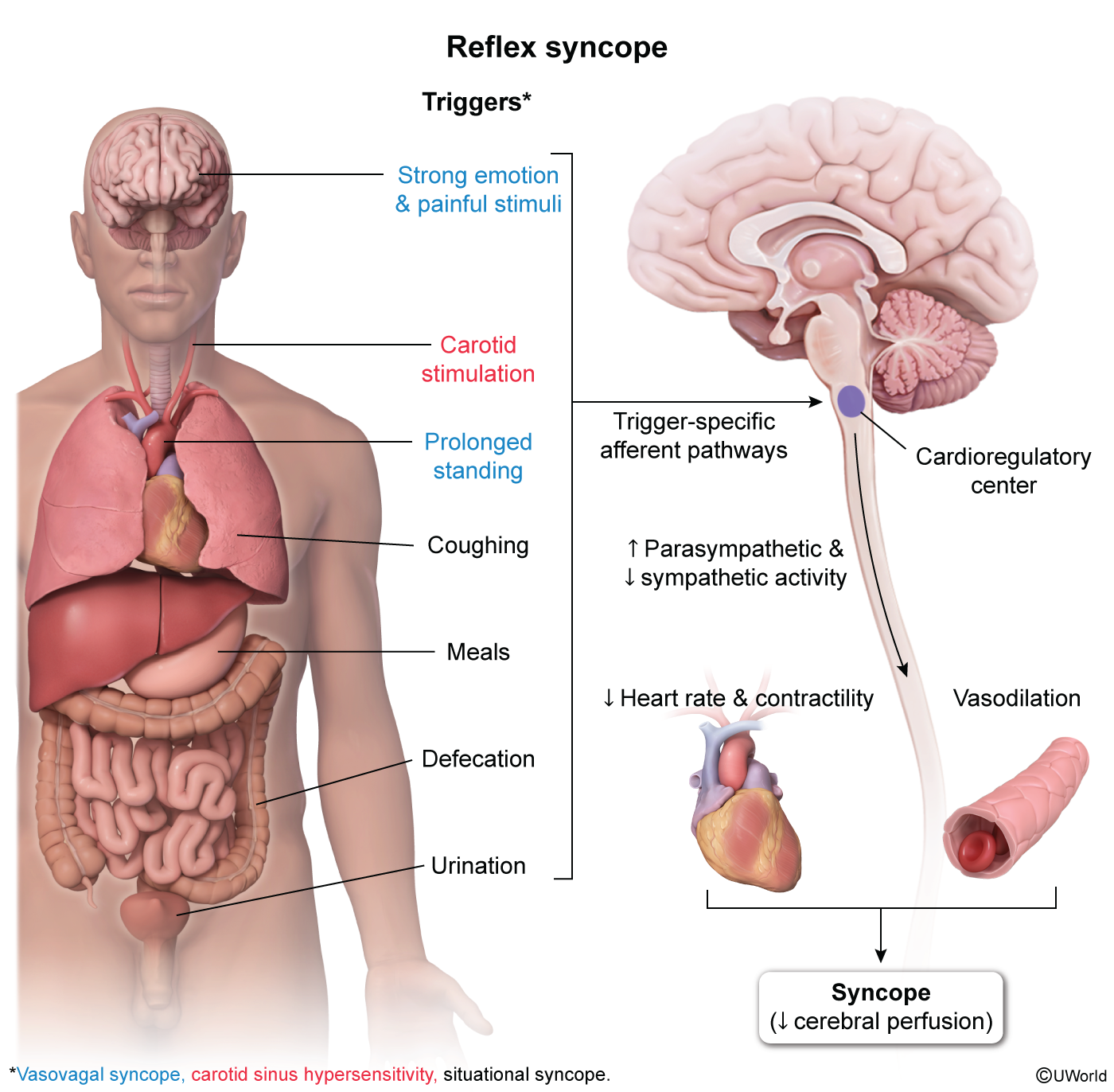
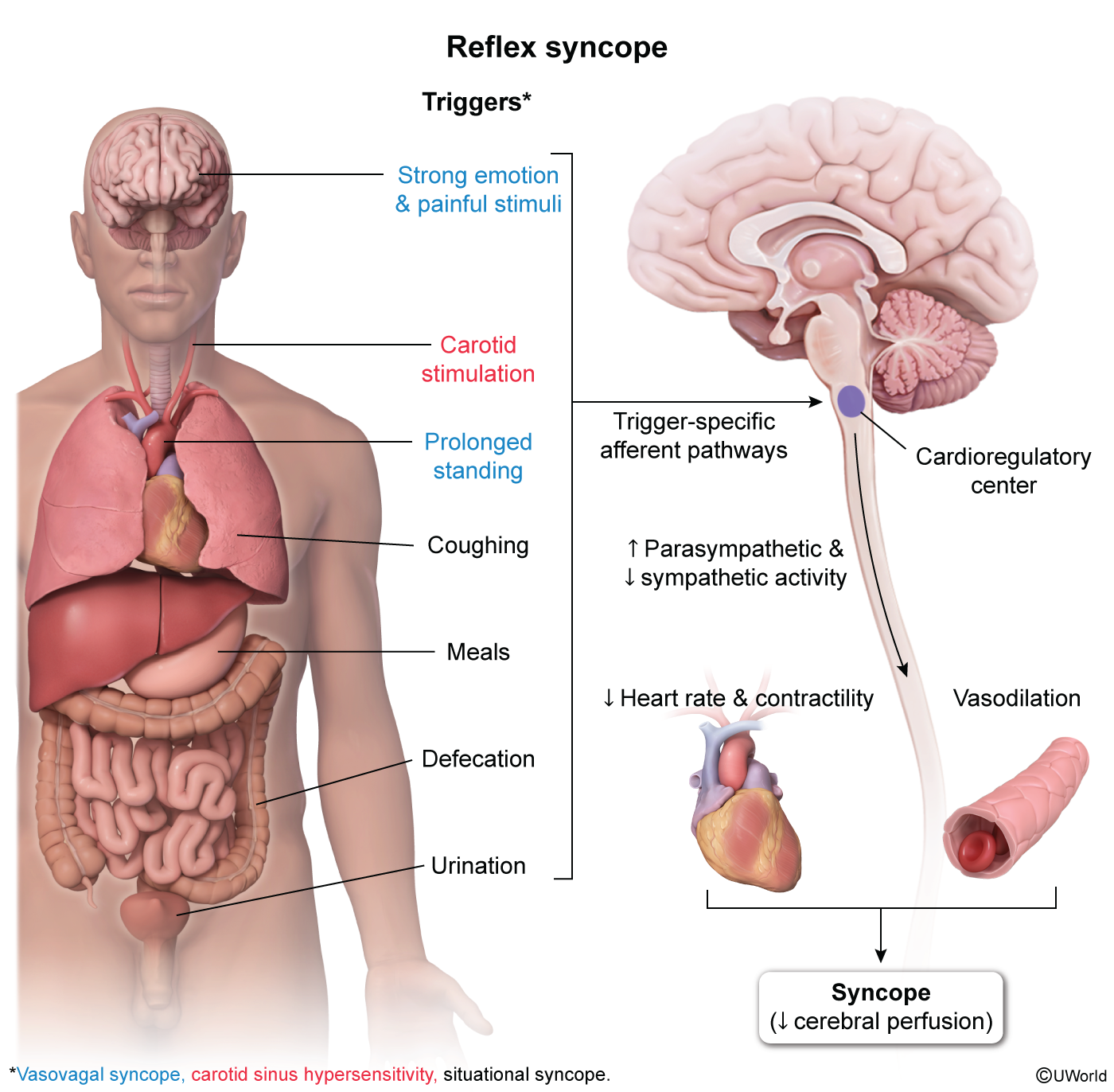
- Reflex (Neurally-Mediated) Syncope: The most common cause, especially in younger individuals.
- Vasovagal: Triggered by stress, fear, pain, or prolonged standing. Involves a cardioinhibitory (vagal-mediated bradycardia) and/or vasodepressor (sympathetic withdrawal leading to vasodilation) response.
- Situational: Occurs with specific triggers like coughing, micturition, defecation, or swallowing.
- Carotid Sinus Hypersensitivity: Triggered by pressure on the carotid sinus (e.g., tight collar, shaving).
- Orthostatic Hypotension: Drop in BP upon standing (↓ SBP >20 mmHg or DBP >10 mmHg).
- Causes include volume depletion (hemorrhage, dehydration), medications (e.g., diuretics, alpha-blockers, antihypertensives), and autonomic dysfunction (e.g., Parkinson’s, diabetes).
- Cardiac Syncope: Most concerning etiology due to high risk of sudden death.
- Clinical Presentation:
- Reflex (Vasovagal): Often preceded by a prodrome (nausea, diaphoresis, warmth, pallor, blurred vision). Typically occurs with a known trigger.
- Orthostatic: Occurs after standing up. History of volume loss or offending medications.
- Cardiac: Often sudden onset without a prodrome. Can be precipitated by exertion (suggests outflow obstruction like AS/HCM) or occur at rest (suggests arrhythmia). Family history of sudden cardiac death is a major red flag.
- Diagnosis:
- Initial Evaluation (All Pts): Thorough history, physical exam (including orthostatic vitals), and a 12-lead ECG.
- ECG: Look for arrhythmias, evidence of prior MI (Q waves), ventricular hypertrophy, Brugada syndrome, prolonged/short QT, or WPW (delta wave).
- Orthostatic Vitals: Positive if SBP drops >20 mmHg, DBP drops >10 mmHg, or HR increases >20 bpm upon standing.
- Further Testing (if indicated):
- Echocardiogram: To evaluate for structural heart disease if murmur or ECG abnormality is present.
- Ambulatory ECG Monitoring (Holter, event recorder): For suspected arrhythmic cause.
- Tilt-table test: To confirm vasovagal syncope if the diagnosis is uncertain.
- Electrophysiology Study (EPS): For high-risk patients with suspected tachyarrhythmia.
- DDx (of Transient Loss of Consciousness):
- Seizure: Key differentiators include a post-ictal state (confusion, drowsiness), lateral tongue biting c , and prolonged tonic-clonic movements. Syncope has a rapid return to baseline.
- During the tonic phase, forceful jaw contraction often causes the patient to bite the lateral aspect of the tongue.
- While tongue biting can occur in syncope (rare), it is typically at the tip of the tongue due to impact with the floor/chin during a fall, rather than the lateral aspect caused by muscle contraction.
- Hypoglycemia: Requires metabolic workup (glucose check).
- Stroke/TIA: Usually associated with focal neurologic deficits. Vertebrobasilar insufficiency can cause syncope.
- Mechanical Fall: No true loss of consciousness.
- Management/Treatment:
- Reflex (Vasovagal): Patient education on avoiding triggers. Counter-pressure maneuvers (e.g., leg crossing, hand gripping) during prodrome.
- Orthostatic Hypotension: Replete volume, adjust offending medications, advise slow postural changes.
- Cardiac: Treat the underlying cause.
- Arrhythmia: Pacemaker for bradycardia, ICD for life-threatening ventricular arrhythmias.
- Structural: e.g., Aortic valve replacement for severe AS.
- Key Associations/Complications (RED FLAGS for Cardiac Syncope):
- Syncope during exertion.
- No prodromal symptoms.
- Abnormal ECG.
- Personal history of structural heart disease or MI.
- Family history of sudden cardiac death at a young age.
- Associated chest pain or shortness of breath.