Etiology
- Primary: Autonomous overproduction of Parathyroid Hormone (PTH).
- Most common cause: Parathyroid adenoma (~85%).
- Other causes: Parathyroid hyperplasia (~15%), parathyroid carcinoma (<1%).
- Associated with MEN 1 and MEN 2A syndromes.
- Secondary: Compensatory PTH secretion due to chronic hypocalcemia.
- Most common cause: Chronic kidney disease (CKD), which leads to decreased 1,25-(OH)2 vitamin D production and hyperphosphatemia.
- Other causes: Severe vitamin D deficiency, malabsorption.
- Tertiary: Autonomous PTH secretion after prolonged secondary hyperparathyroidism.
- The parathyroid glands become hyperplastic and no longer respond to normal feedback mechanisms.
- Typically seen in patients with end-stage renal disease (ESRD), often after a renal transplant.
Parathyroid function
- Bone: Increases bone resorption by indirectly activating osteoclasts (via RANKL on osteoblasts), releasing Ca2+ and PO4(3-).
- Kidney: Increases Ca2+ reabsorption in the distal convoluted tubule. Decreases PO4(3-) reabsorption in the proximal convoluted tubule (“Phosphate trashing”). Stimulates 1-alpha-hydroxylase to convert 25-hydroxyvitamin D to active 1,25-dihydroxyvitamin D (calcitriol).
- Gut: Active Vitamin D increases intestinal absorption of both Ca2+ and PO4(3-).
Clinical features
Symptomatic patients often have clinical features of hypercalcemia
Clinical features
- Nephrolithiasis, nephrocalcinosis (calcium oxalate > calcium phosphate stones)
- Bone pain, arthralgias, myalgias, fractures
- Because most of the calcium is released from bones
- Constipation
- Increase in extracellular Ca2+ → membrane potential outside is more positive → more amount of depolarization is needed to initiate action potential → decreased excitability of muscle and nerve tissue
- Abdominal pain
- Nausea and vomiting
- Anorexia
- Peptic ulcer disease
- hypercalcemia-induced increase of gastric acid secretion and gastrin levels.
- Neuropsychiatric symptoms such as anxiety, depression, fatigue, and cognitive dysfunction
- Diminished muscle excitability
- Cardiac arrhythmias
- ECG: Shorten QT interval, see QT interval
- Muscle weakness, paresis
- Polyuria and dehydration
- Due to acquired renal ADH resistance. Although ADH is being secreted, the kidneys no longer respond to it adequately (nephrogenic diabetes insipidus).
Link to original
Diagnostics
- Labs
- Primary hyperparathyroidism: ↑ Serum Ca2+, ↑ PTH, ↓ Serum PO₄³⁻, ↑ Urinary Ca2+, ↑ Urinary cAMP
- The severe hypercalcemia overwhelms the kidney’s ability to reabsorb calcium, resulting in a net increase in urinary calcium (hypercalciuria).
- PTH acts on the kidney via a Gs-coupled receptor, which increases cAMP. This cAMP is then excreted, leading to ↑ Urinary cAMP.
- Primary hyperparathyroidism: ↑ Serum Ca2+, ↑ PTH, ↓ Serum PO₄³⁻, ↑ Urinary Ca2+, ↑ Urinary cAMP
- Neck imaging
- For surgical planning to determine the location of the abnormal glands and evaluate for concomitant thyroid disease
- Options include ultrasound neck and nuclear imaging, i.e., Tc-99m sestamibi scan.
- X-ray
- Decreased bone mineral density
- Cortical thinning: especially prominent in the phalanges of the hand; manifests as acroosteolysis (a subperiosteal pattern of bone resorption)
- Unlike the typical osteoporosis of aging, which predominantly affects trabecular bone
- Salt and pepper skull: granular decalcification manifesting as diffusely distributed lytic foci on imaging of the calvarium
- Features of osteitis fibrosa cystica
Complications
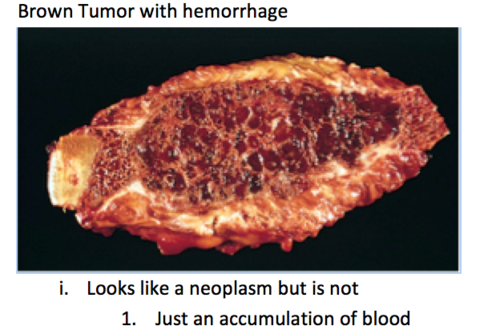
Osteitis fibrosa cystica (OFC)
- A rare skeletal disorder seen in advanced hyperparathyroidism characterized by replacement of calcified bone with fibrous tissue
- Most commonly seen in primary hyperparathyroidism but can also occur in secondary hyperparathyroidism
- ↑ PTH → ↑ RANK ligand expression → activation of osteoclasts → bone resorption, cortical bone destruction, and fibrous tissue deposition
- Features include bone pain, subperiosteal thinning, and bone cysts; multiple bone cysts in the skull may result in a salt and pepper skull (pepper pot) appearance on x-ray.
- In advanced OFC, large, cystic, vascular cavities with a tumor-like appearance on x-ray and a brown color due to hemosiderin deposition (brown tumors) can form in long bones.