Epidemiology
Etiology
Pathophysiology
- Tumor classification according to ability to secrete hormones
- Nonsecretory pituitary adenomas
- Nonfunctioning tumors account for 15–45% of all pituitary adenomas.
- Gonadotroph adenomas
- Null cell adenomas
- Plurihormonal adenomas
- Silent somatotroph and corticotroph adenomas
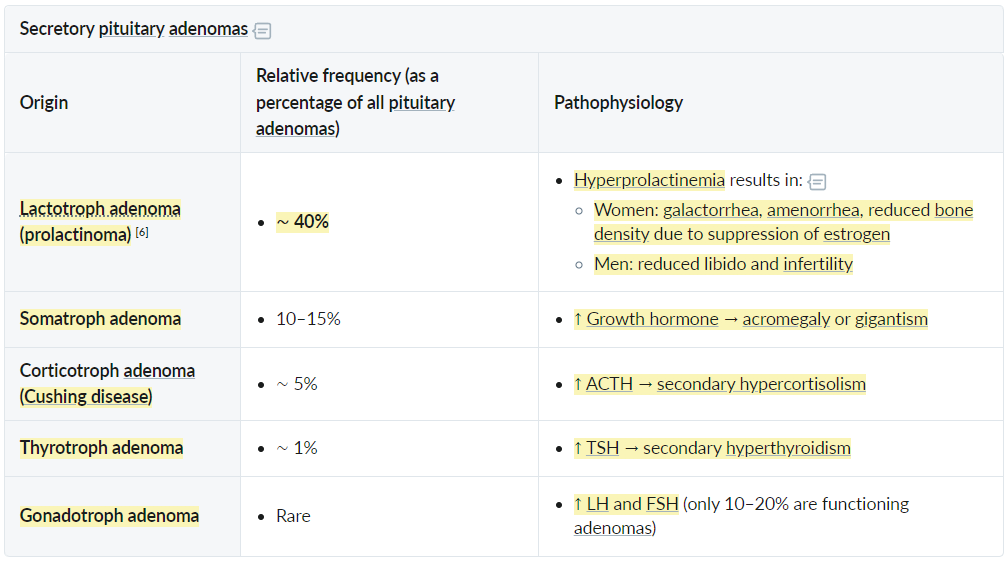
- Secretory pituitary adenomas: hormone secretion → hyperpituitarism
- Most exclusively proliferate in only one type of endocrine cell and therefore secrete only one pituitary hormone.
- Nonsecretory pituitary adenomas
Tip
Prolactinomas are the most common pituitary adenomas.
Subtypes
- Prolactinoma (Most Common)
- Pathophysiology: Hypersecretion of Prolactin → inhibition of GnRH.
- Sx (Women): Galactorrhea, amenorrhea/oligomenorrhea, infertility.
- Sx (Men): ↓ Libido, erectile dysfunction, gynecomastia (often caught later as macroadenoma).
- Growth Hormone (GH) Adenoma (Somatotroph)
- Children: Gigantism (linear growth before epiphyseal closure).
- Adults: Acromegaly (coarse facial features, enlarging hands/feet/hat size, macroglossia, prognathism).
- Complications: Cardiomyopathy (HF), Colorectal polyps/cancer, Diabetes (GH induces insulin resistance).
- ACTH Adenoma (Corticotroph)
- Causes Cushing Disease.
- Sx: Weight gain, moon facies, buffalo hump, striae, HTN, hyperglycemia.
- Gonadotroph Adenoma (FSH/LH)
- Usually non-functional/silent.
- Present with mass effect.
Clinical features
- Mass Effect (especially Macroadenomas >1 cm):
- Headaches are a common symptom.
- Bitemporal hemianopsia: Classic visual field defect due to compression of the optic chiasm.
- Cranial nerve palsies from invasion of the cavernous sinus (CN III, IV, V1, V2, VI).
- Hypopituitarism: Compression of normal pituitary tissue leading to hormone deficiencies (e.g., hypothyroidism, hypogonadism).
Diagnostics
Treatment
- Prolactinoma:
- Dopamine agonists (e.g., Cabergoline, Bromocriptine) are first-line therapy. They decrease prolactin levels and shrink the tumor.
- Transsphenoidal surgery is reserved for patients who do not respond to or cannot tolerate medical therapy.
- Acromegaly & Cushing’s Disease:
- Transsphenoidal surgery is the primary treatment.
- Medical therapy can be used adjunctively. For acromegaly, options include somatostatin analogs (e.g., Octreotide) or GH receptor antagonists (e.g., Pegvisomant). For Cushing’s, adrenal enzyme inhibitors (e.g., Ketoconazole) can be used.
- Radiation therapy may be used for residual or recurrent tumors.
- Non-functioning Adenoma:
- Observation for small, asymptomatic tumors.
- Transsphenoidal surgery if mass effect symptoms (e.g., vision changes) are present.
Complications
Pituitary apoplexy
- Etiology/Pathophysiology
- Sudden hemorrhage or infarction of a pre-existing pituitary adenoma.
- Often the first clinical presentation of a previously undiagnosed adenoma.
- The rapid expansion of the sellar mass leads to compression of surrounding structures (optic chiasm, cavernous sinus) and acute pituitary dysfunction.
- Clinical Features
- Classic Triad:
- Sudden, severe headache (“thunderclap headache”).
- Visual field defects (classically bitemporal hemianopsia from optic chiasm compression).
- Ophthalmoplegia (diplopia due to CN III, IV, VI palsies from cavernous sinus invasion).
- Signs of meningeal irritation (nuchal rigidity) due to blood in the subarachnoid space.
- Altered mental status, nausea/vomiting.
- Features of acute panhypopituitarism, which is the most life-threatening aspect:
- Acute adrenal insufficiency (secondary): Hypotension, shock, hypoglycemia, fever. This is a medical emergency.
- Central hypothyroidism: Can contribute to altered mental status.
- Classic Triad:
- Diagnostics
- Initial Imaging: Non-contrast head CT is often done first to rule out subarachnoid hemorrhage. May show a hyperdense sellar mass.
- Definitive Imaging: MRI of the pituitary is the gold standard; shows hemorrhage and necrosis within the adenoma.
- Labs (Urgent):
- Assess for acute adrenal insufficiency: ↓ cortisol, ↓ ACTH.
- Evaluate other pituitary axes: TSH, free T4, prolactin, LH, FSH.
- Check electrolytes: Hyponatremia is common due to cortisol deficiency (impaired free water excretion) or SIADH.
- Treatment
- This is a NEUROENDOCRINE EMERGENCY.
- 1st Step: Administer high-dose glucocorticoids (e.g., IV hydrocortisone or dexamethasone) immediately. Do NOT wait for imaging or lab confirmation if clinically suspected. This treats the life-threatening adrenal crisis.
- Supportive Care: IV fluids, electrolyte correction.
- Neurosurgical Consultation: Urgent decompression via transsphenoidal surgery is indicated for:
- Progressive visual deterioration.
- Severe or persistent ophthalmoplegia.
- Declining level of consciousness.
- Complications & Prognosis
- Permanent hypopituitarism is common, requiring lifelong hormone replacement (e.g., levothyroxine, cortisol, sex steroids).
- Mortality is high if acute adrenal insufficiency is not promptly treated.
- Vision may not fully recover.