Epidemiology
Etiology
Hypercortisolism can be categorized as either ACTH-dependent or ACTH-independent.
- ACTH-Dependent Causes:
- Cushing’s Disease: This is the most common endogenous cause, resulting from an ACTH-secreting pituitary adenoma.
- Ectopic ACTH Syndrome: Non-pituitary tumors, most commonly small-cell lung cancer, can secrete ACTH.
- ACTH-Independent Causes:
- Iatrogenic (Exogenous): This is the most common overall cause, resulting from long-term administration of glucocorticoid medications.
- Adrenal Tumors: Adrenal adenomas or carcinomas can autonomously produce excess cortisol.
Pathophysiology
Clinical features
Mnemonic
诱发三高和溃疡,伤口感染不好长,骨松眼青人发狂 三高 is related to Permissive action of corticosteroids
“CUSHINGOID”
- Central obesity, Cervical fat pad (Buffalo hump), Collagen weakness.
- Urinary free cortisol ↑.
- Striae (purple/violaceous, typically >1 cm wide), Skin thinning, easy bruising.
- Hypertension, Hirsutism, Hyperglycemia (insulin resistance).
- Immunosuppression (↑ risk of infections).
- Neoplasia.
- Glucose intolerance/Diabetes.
- Osteoporosis (risk of fractures), Oligomenorrhea/Amenorrhea.
- Immunosuppression.
- Depression/Psychiatric symptoms (anxiety, irritability).
- Moon facies: Rounded, plethoric face due to fat deposition.
- Proximal muscle weakness: Due to cortisol’s catabolic effect on muscle.
- ↑ Hematocrit
- Steroids, particularly anabolic steroids, stimulate the production of erythropoietin
Diagnostics
-
Confirm Hypercortisolism: Initial screening tests are used to confirm the presence of excess cortisol. These include:
- 24-hour urinary free cortisol (UFC)
- Late-night salivary cortisol
- Low-dose dexamethasone suppression test
- Screening test only
- In a healthy person, giving a low dose of dexamethasone (a potent steroid) will suppress the pituitary’s ACTH production, causing morning cortisol levels to be low.
- In a patient with Cushing’s syndrome, the source of cortisol is autonomous and will not be suppressed by a low dose. Their morning cortisol will remain high.
-
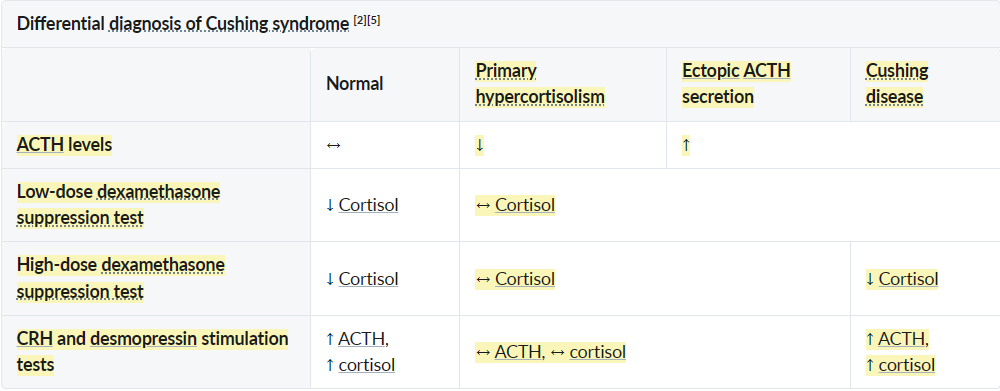
Determine Etiology: Once hypercortisolism is confirmed, plasma ACTH levels are measured to differentiate between ACTH-dependent and ACTH-independent causes.
- Low ACTH: Suggests an adrenal source (adenoma or carcinoma).
- Normal or High ACTH: Indicates an ACTH-dependent cause (pituitary or ectopic).
-
Localize the Source:
- If ACTH is low, a CT or MRI of the adrenal glands is performed.
- If ACTH is high, a high-dose dexamethasone suppression test and/or a CRH stimulation test can help distinguish between a pituitary source (Cushing’s disease) and an ectopic source. An MRI of the pituitary is the next step for suspected Cushing’s disease.
- Most pituitary adenomas retain partial sensitivity to feedback inhibition in response to high doses of glucocorticoids, while ectopic tumors are resistant even to high doses.
Treatment
Bilateral adrenalectomy
- Indications
- Primary hypercortisolism caused by bilateral adrenal disease (recommended curative treatment)
- Emergency treatment in severe ACTH-dependent hypercortisolism that cannot be controlled pharmacologically
- Symptomatic treatment for metastatic or occult ectopic tumors
- Complication: Nelson syndrome (post adrenalectomy syndrome)
- Etiology: bilateral adrenalectomy in patients with a previously undetected pituitary adenoma
- Pathophysiology: bilateral adrenalectomy → no endogenous cortisol production → no negative feedback from cortisol on the hypothalamus → ↑ CRH production → uncontrolled enlargement of preexisting but undetected ACTH-secreting pituitary adenoma → ↑ secretion of ACTH and MSH → manifestation of symptoms due to pituitary adenoma and ↑ MSH
- Clinical features: headache, bitemporal hemianopia (mass effect), cutaneous hyperpigmentation
- Diagnostics
- High levels of β-MSH and ACTH
- Pituitary adenoma on MRI confirms the diagnosis.
- Treatment: surgery (e.g., transsphenoidal resection) and/or pituitary radiation therapy (e.g., if the tumor cannot be fully resected)