General Principles
- Visual Pathway: Retina → Optic Nerve → Optic Chiasm → Optic Tract → Lateral Geniculate Nucleus (LGN) of Thalamus → Optic Radiations → Primary Visual Cortex (Occipital Lobe).
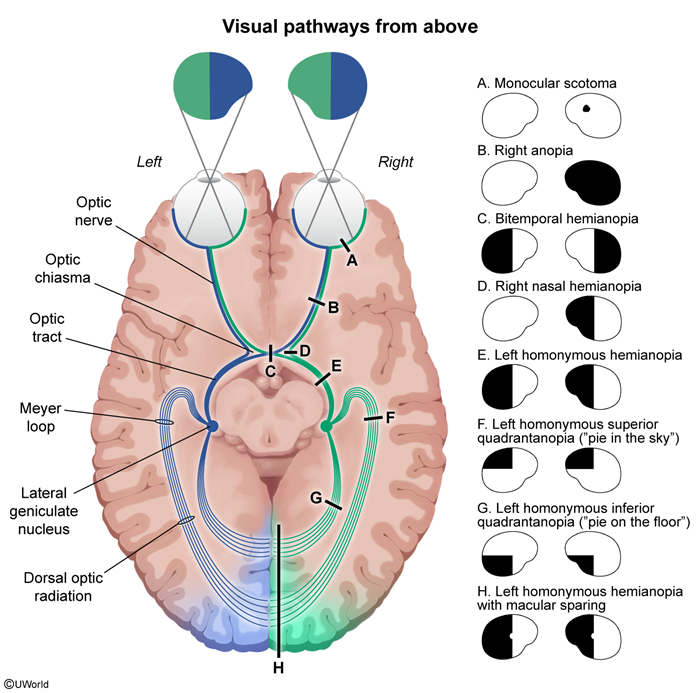
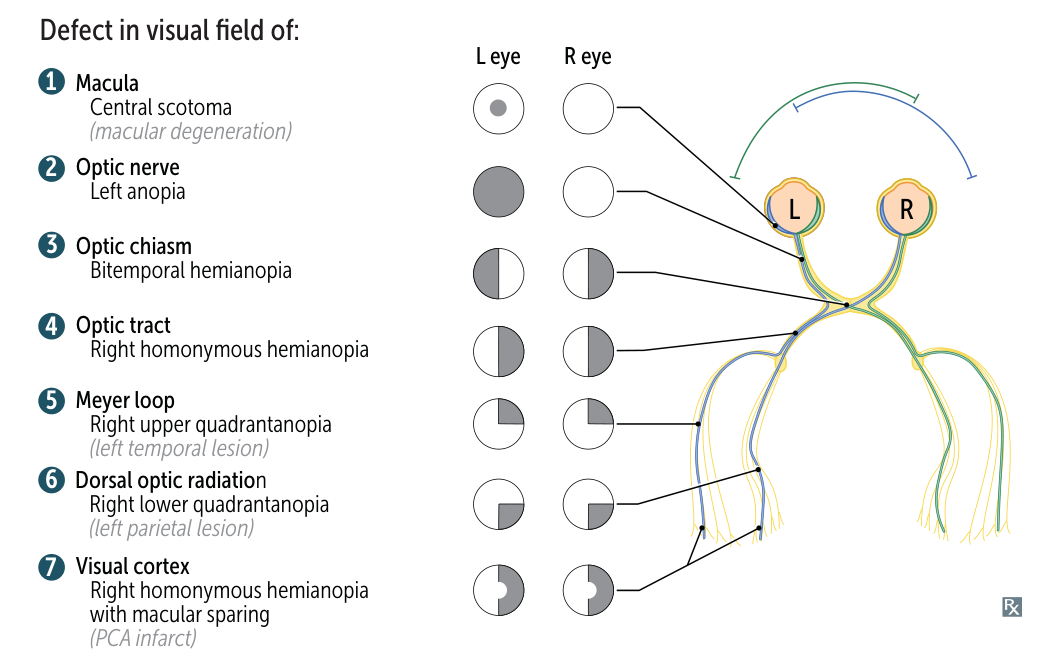
- Rule of Thumb: Pre-chiasmal lesions cause ipsilateral, monocular defects. Post-chiasmal (retrochiasmal) lesions cause contralateral, homonymous (affecting the same side of the visual field in both eyes) defects.
- Information from the right visual field projects to the left hemisphere, and vice-versa.
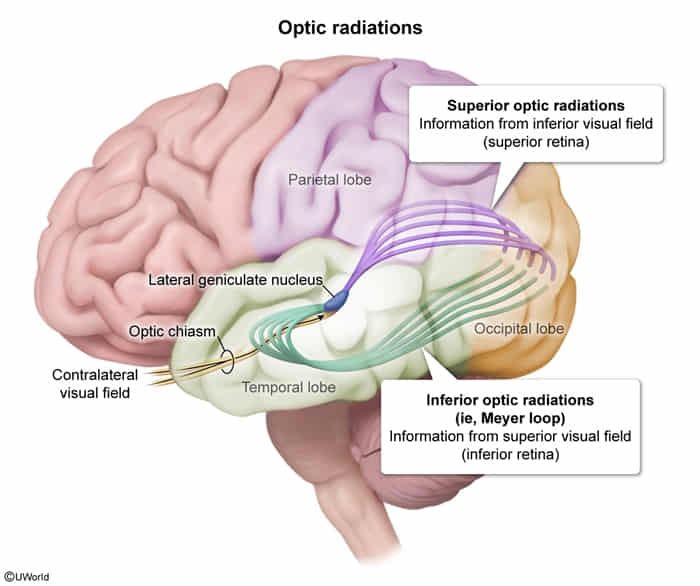
- Information from the superior visual field projects to the inferior retina and then to the inferior optic radiations (Meyer’s loop) and inferior calcarine sulcus.
- Information from the inferior visual field projects to the superior retina and then to the superior optic radiations (Baum’s loop/parietal) and superior calcarine sulcus.
Lesion Locations & Corresponding Defects
-
Optic Nerve
- Defect: Ipsilateral monocular blindness (anopia) or scotoma (localized blind spot).
- Etiology: Optic neuritis (e.g., multiple sclerosis), glaucoma, retinal artery/vein occlusion, trauma, tumor.
- Key Finding: Relative Afferent Pupillary Defect (RAPD) or Marcus Gunn pupil on swinging-flashlight test.
-
Optic Chiasm
- Defect (Central Lesion): Bitemporal hemianopia. Loss of the outer (temporal) visual fields in both eyes.
- Etiology: Pituitary adenoma (most common), craniopharyngioma, suprasellar meningioma, aneurysm of the anterior communicating artery.
- Defect (Lateral/Junctional Lesion):
- Junctional Scotoma of Traquair: Ipsilateral temporal hemianopic defect due to compression of ipsilateral nasal crossing fibers at the nerve-chiasm junction.
- Junctional Scotoma: Ipsilateral optic neuropathy (e.g., central scotoma) plus a contralateral superior temporal defect (“pie in the sky”) due to compression of inferonasal fibers from the opposite eye (Wilbrand’s Knee) crossing into the optic nerve before decussating.
-
Optic Tract
- Defect: Contralateral homonymous hemianopia.
- Etiology: Stroke (anterior choroidal artery), tumor, trauma.
- Note: Defects are often incongruous (asymmetric between the two eyes) because fibers from corresponding retinal points are not yet perfectly aligned.
-
Optic Radiations (Geniculocalcarine Tract)
- Meyer’s Loop (Temporal Lobe):
- Defect: Contralateral superior homonymous quadrantanopia (“pie in the sky”).
- Etiology: Stroke (MCA territory), temporal lobe tumors, anterior temporal lobe resection for epilepsy.
- Baum’s Loop (Parietal Lobe):
- Defect: Contralateral inferior homonymous quadrantanopia (“pie on the floor”).
- Etiology: Stroke (MCA territory), parietal lobe tumors.
- Associated Signs: If in the dominant (usually left) parietal lobe, may see Gerstmann syndrome (agraphia, acalculia, finger agnosia, right-left disorientation). If non-dominant, may see contralateral hemineglect.
- Meyer’s Loop (Temporal Lobe):
-
Visual Cortex (Occipital Lobe)
- Defect: Contralateral homonymous hemianopia with macular sparing.
- Etiology: Posterior Cerebral Artery (PCA) stroke is the classic cause.
- Macular Sparing: The macula (central vision) has a dual blood supply from both the MCA and PCA, so a PCA occlusion may spare the occipital pole where macular fibers terminate.
- Temporal Crescent Defect: A lesion to the most anterior part of the visual cortex can cause a monocular visual field loss in the contralateral eye’s far temporal periphery.