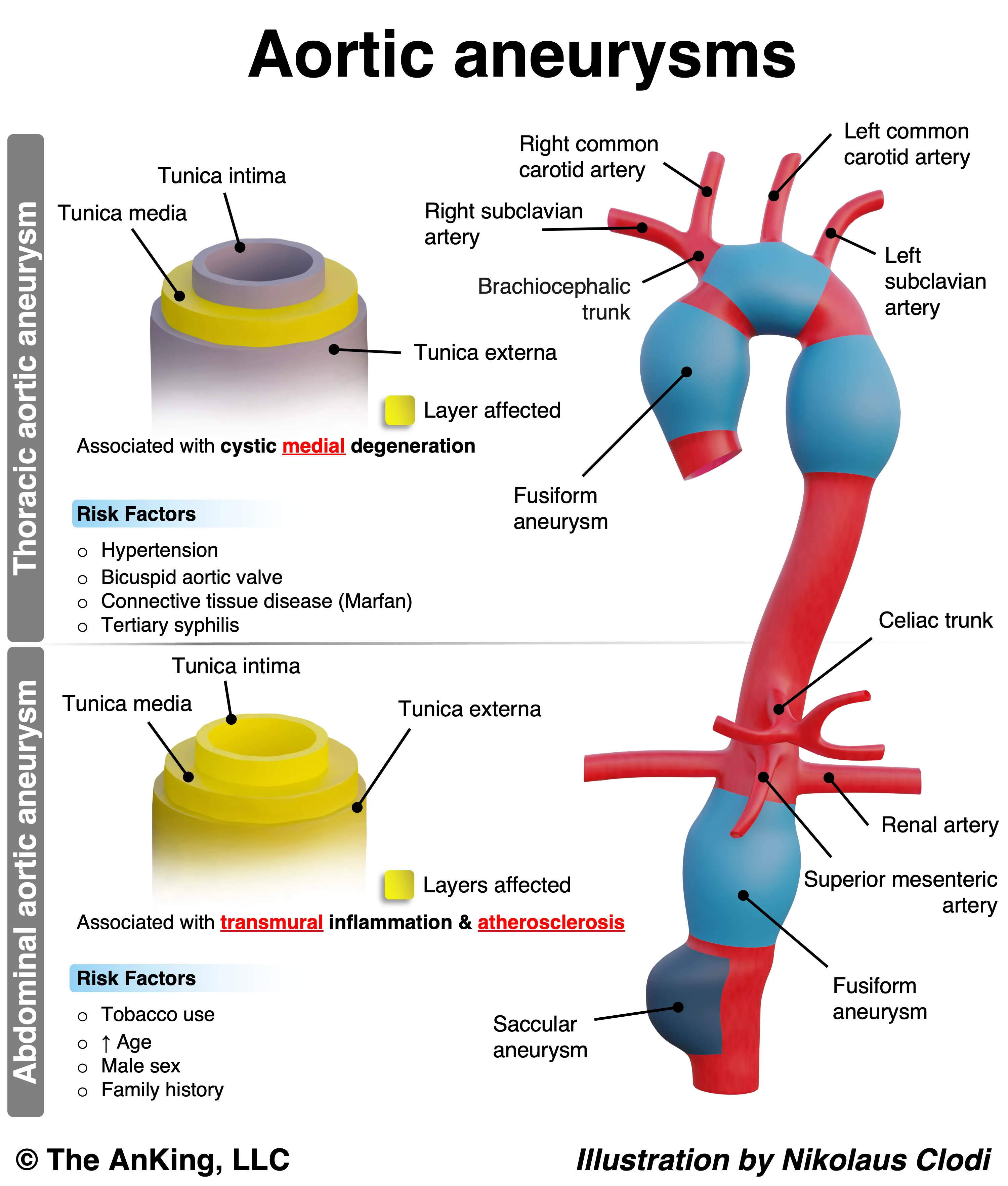
Abdominal Aortic Aneurysm (AAA)
- Etiology/Pathophysiology
- Most common true arterial aneurysm.
- Primary cause: Atherosclerosis, leading to chronic inflammation, elastin degradation, and weakening of the aortic wall.
- Location: Almost always infrarenal (below the renal arteries), partly due to the absence of vasa vasorum in this segment, making it more susceptible to ischemia.
- Defined as aortic diameter > 3.0 cm.
- Risk Factors
- Smoking: Strongest modifiable risk factor.
- Age > 60-65 years.
- Male gender (4:1 ratio).
- Family history.
- Hypertension.
- Clinical Features
- Diagnostics
- Screening/Initial Dx: Abdominal ultrasound.
- USPSTF recommends a one-time screening for men aged 65-75 who have ever smoked.
- Pre-operative planning/Symptomatic pts: CT angiography is the test of choice for detailed anatomical mapping.
- Screening/Initial Dx: Abdominal ultrasound.
- Treatment
- Conservative management for aneurysms < 5.5 cm:
- Smoking cessation.
- BP control (e.g., beta-blockers).
- Serial ultrasound monitoring.
- Surgical Repair: Indicated if:
- Diameter > 5.5 cm in men or > 5.0 cm in women.
- Rapid growth (>0.5 cm in 6 months or >1 cm per year).
- Presence of symptoms or rupture.
- Options: Open repair or Endovascular Aneurysm Repair (EVAR).
- Conservative management for aneurysms < 5.5 cm:
Thoracic Aortic Aneurysm (TAA)
- Etiology/Pathophysiology
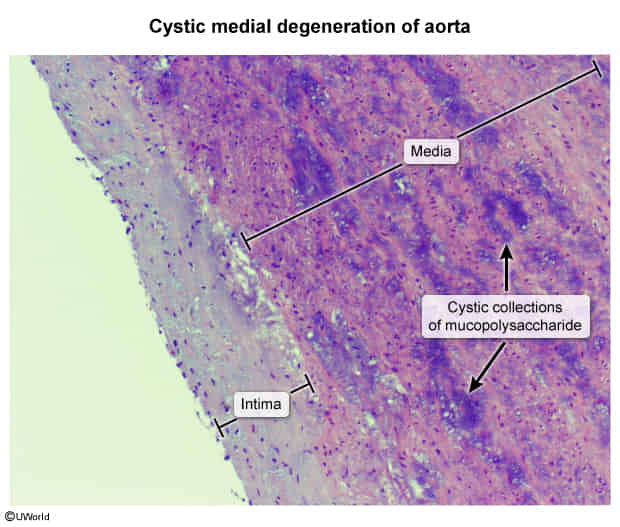
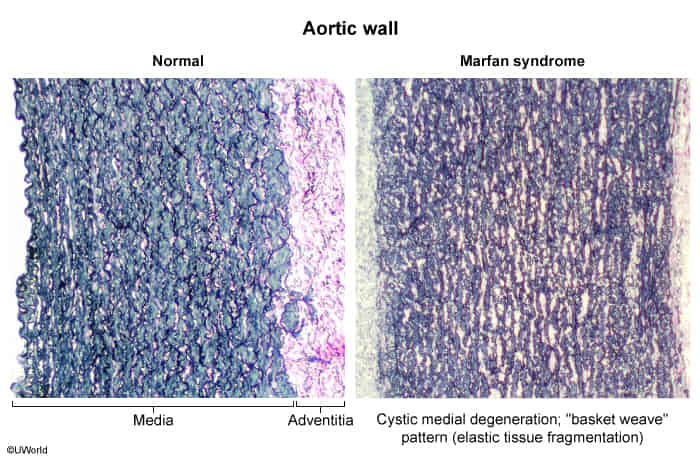
- Primary cause: Cystic medial necrosis, a degenerative process of the aortic media.
- It is characterized by the breakdown and loss of the structural components that give the aortic wall its strength and elasticity.
- This loss of structural elements leads to the formation of small, empty spaces or “cysts” that fill with a basophilic, mucopolysaccharide-rich substance (mucoid material).
- Associated Conditions:
- Connective tissue diseases: Marfan syndrome (FBN1 gene mutation) and Ehlers-Danlos syndrome (collagen defects).
- Bicuspid aortic valve.
- Tertiary syphilis (obliterative endarteritis of the vasa vasorum) → classic “tree-bark” appearance of the aorta.
- Location: Most commonly involves the ascending aorta.
- Primary cause: Cystic medial necrosis, a degenerative process of the aortic media.
- Risk Factors
- Hypertension.
- Connective tissue disorders (Marfan, Ehlers-Danlos).
- Family history.
- Smoking.
- Clinical Features
- Mostly asymptomatic.
- Symptomatic (due to compression of adjacent structures):
- Rupture/Dissection: Presents as sudden, severe, tearing chest pain radiating to the back.
- Diagnostics
- Initial/Incidental Finding: Often seen as a widened mediastinum on chest X-ray.
- Definitive Dx: CT angiography is the gold standard for diagnosis and pre-operative planning.
- Treatment
- Medical management:
- Strict BP control, with beta-blockers being first-line to reduce aortic wall shear stress.
- Activity restriction (e.g., avoiding heavy lifting).
- Surgical Repair: Indicated if:
- Diameter > 5.5-6.0 cm for ascending aorta.
- Diameter > 5.0 cm in patients with Marfan syndrome.
- Rapid growth.
- Presence of symptoms or dissection.
- Options: Open surgical repair or Thoracic Endovascular Aortic Repair (TEVAR).
- Medical management:
| Feature | Abdominal Aortic Aneurysm (AAA) | Thoracic Aortic Aneurysm (TAA) | Aortic Dissection |
|---|---|---|---|
| Patho | True aneurysm; Wall weakening | True aneurysm; Wall weakening | Intimal tear, false lumen |
| Location | Infrarenal | Ascending or Descending | Stanford A (Ascending), B (Descending) |
| #1 Risk Factor | Atherosclerosis (Smoking) | Hypertension / Marfan | Hypertension |
| Presentation | Usually asymptomatic, pulsatile mass | Usually asymptomatic, compression Sx | Tearing chest pain radiating to back |
| Key Finding | Pulsatile abdominal mass | Aortic regurgitation murmur | Asymmetric BPs or pulses |
| Dx | Ultrasound (screening) | CT Angiography (CTA) | CTA (stable), TEE (unstable) |
| Tx | Repair if >5.5 cm or symptomatic | Repair if >5.5 cm or symptomatic | A: Surgery B: Medical (β-blockers) |