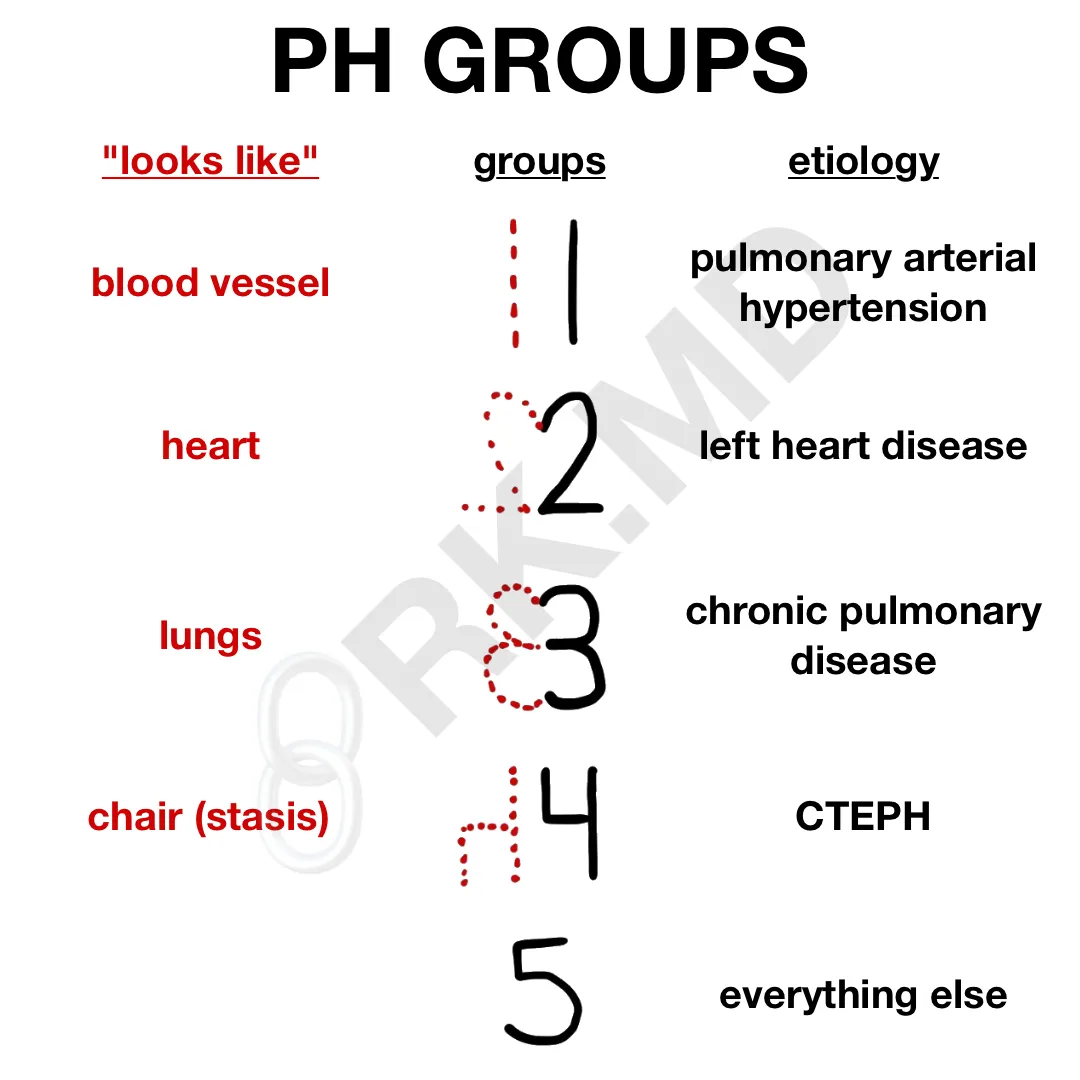
Epidemiology
Etiology
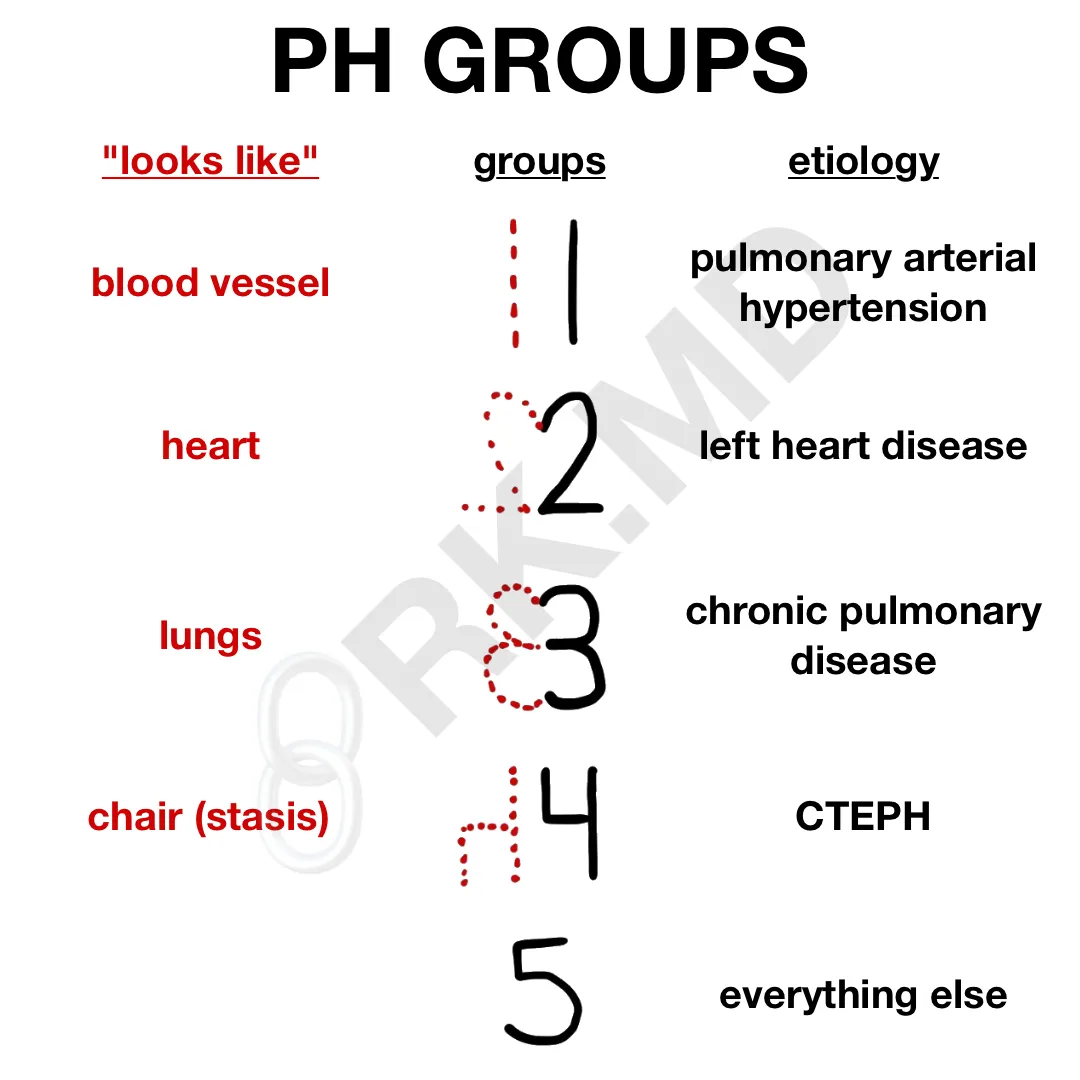
- Group 1: Pulmonary Arterial Hypertension (PAH)
- Precapillary PH due to structural changes in small pulmonary arterioles (vasoconstriction, remodeling, thrombosis).
- Subtypes:
- Idiopathic (most common cause of PAH).
- Heritable: Associated with an inactivating mutation in the BMPR2 gene, which normally inhibits vascular smooth muscle proliferation.
- Associated with: Connective tissue diseases (e.g., scleroderma), HIV infection, portal hypertension, congenital heart disease, and schistosomiasis.
- Drug/Toxin-induced: Amphetamines, cocaine.
- Group 2: PH due to Left Heart Disease
- Most common cause of PH overall.
- Due to backward pressure from left-sided heart failure (systolic or diastolic) or valvular disease (e.g., mitral stenosis).
- Group 3: PH due to Chronic Lung Disease and/or Hypoxia
- Caused by conditions like COPD, interstitial lung disease (ILD), chronic exposure to high altitude t , or obstructive sleep apnea (OSA).
- Pathophysiology involves hypoxic vasoconstriction.
- Group 4: Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
- Caused by unresolved or recurrent pulmonary emboli leading to obstruction.
- Group 5: PH with Unclear/Multifactorial Mechanisms
- Includes hematologic disorders (e.g., sickle cell), systemic disorders (e.g., sarcoidosis), and metabolic disorders.
Pathophysiology
- ↑ Pulmonary vascular resistance (PVR) is the key mechanism, driven by:
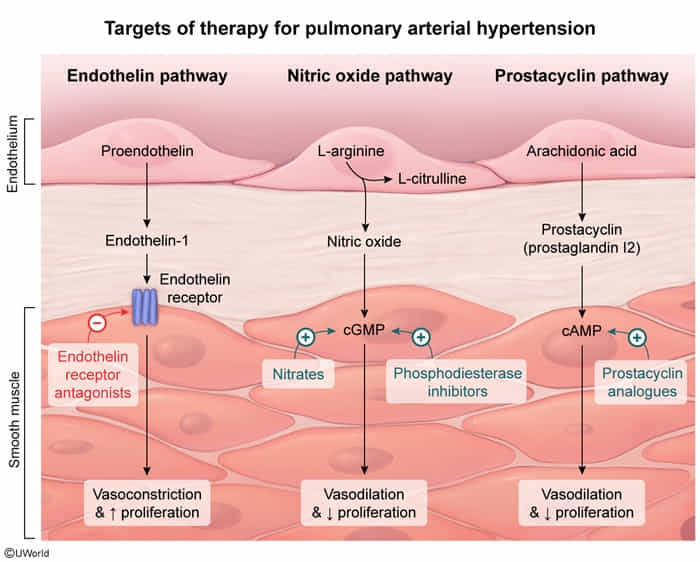
- Vasoconstriction: Imbalance of vasodilators (↓ nitric oxide, prostacyclin) and vasoconstrictors (↑ endothelin).
- Vascular remodeling: Hypertrophy and hyperplasia of intima, media, and adventitia of pulmonary arterioles.
- In-situ thrombosis.
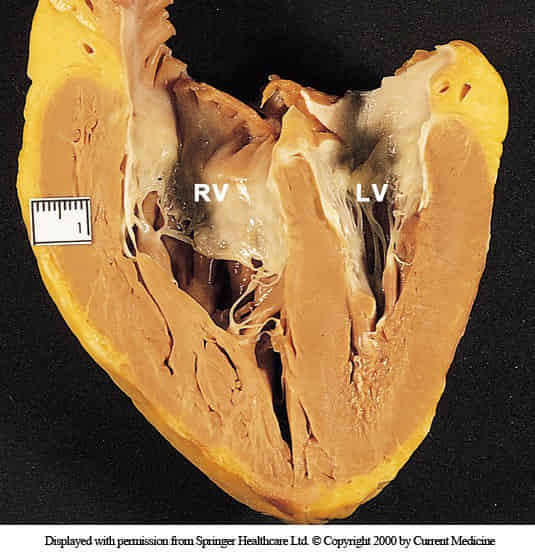
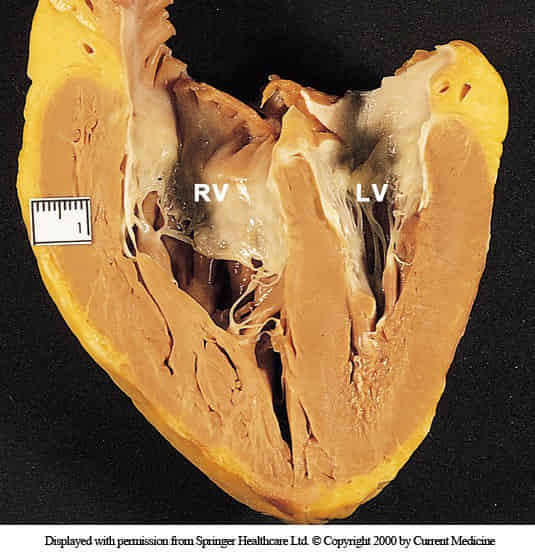
- Increased PVR leads to ↑ afterload on the right ventricle.
- Leads to right ventricular (RV) hypertrophy and subsequent RV dilation and failure (cor pulmonale).
Clinical features
Diagnostics
- Thickening of the right ventricular free wall
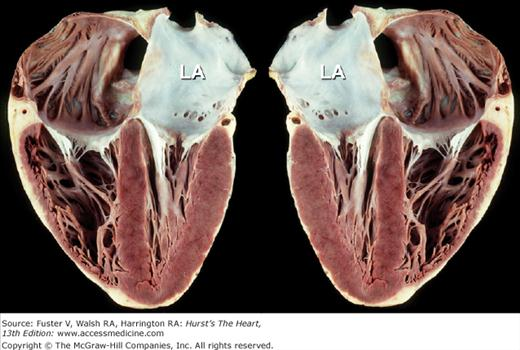
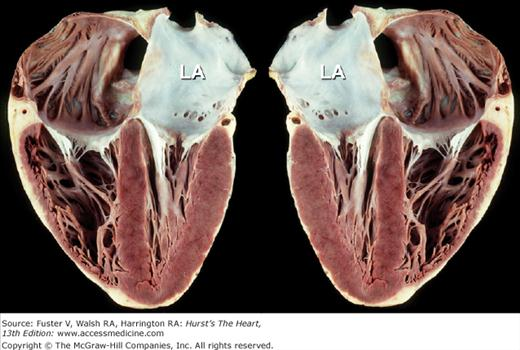
- Normal heart
Treatment
Group 1 PH: PAH
- Calcium channel blockers: First-line pulmonary vasodilator therapy for patients with PAH and positive vasoreactivity testing
- Other pulmonary vasodilator therapies: typically second-line agents, the choice of which depends on symptom severity
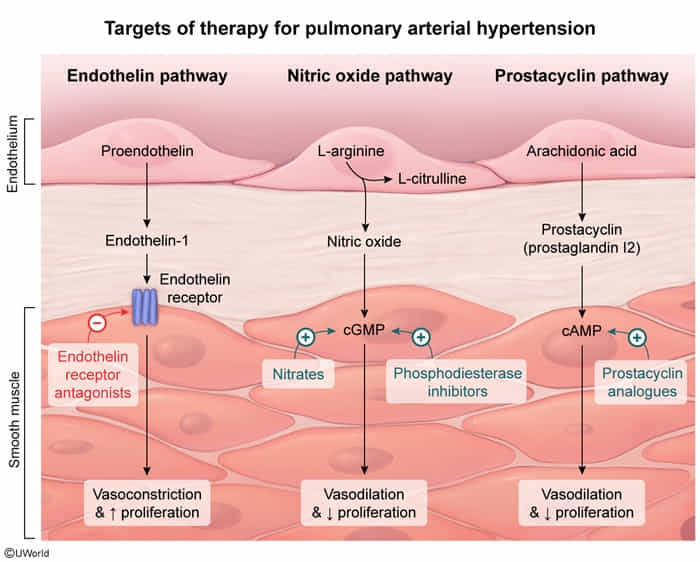
- Endothelin receptor antagonists (e.g., bosentan, macitentan, ambrisentan)
- Competitively inhibit endothelin-1 receptors → ↓ vasoconstriction in the pulmonary circuit
- Phosphodiesterase-5 inhibitors (e.g., sildenafil)
- PDE5 inhibition → ↓ breakdown of cGMP → pulmonary vasodilation, penile smooth muscle relaxation, and ↑ blood flow
- Prostacyclin analogs (iloprost, treprostinil) OR Synthetic prostacyclin (epoprostenol)
- Prostacyclin (PGI2) acts as a direct vasodilator (systemic and pulmonary) and inhibits platelet aggregation via prostacyclin receptors.
- Receptor binding of prostacyclins or prostacyclin analogs → ↑ intracellular cAMP → inhibition of myosin light chain kinase → vascular smooth muscle relaxation
- Group 2: Treat left heart dz.
- Group 3: Treat lung dz + O2 therapy.
- Group 4: Lifelong anticoagulation; surgical pulmonary endarterectomy (curative).
- Severe: Lung transplant.