Epidemiology
Etiology
Predisposing factors
- Nulliparity
- Early menarche (< 10 years of age)
- Age: 25–45 years
- Fibroids are largely found in women of reproductive age.
- Influenced by hormones (i.e., estrogen, growth hormone, and progesterone)
- During menopause, hormone levels begin to decrease and leiomyomas begin to shrink.
- Increased incidence in African American individuals
Pathophysiology
Clinical features
- Symptoms depend on the number, size, and location of leiomyomas. Often asymptomatic (up to 80% of cases).
- Abnormal menstruation (possibly associated with anemia): hypermenorrhea, heavy menstrual bleeding, metrorrhagia, dysmenorrhea
- Submucosal leiomyomas are most frequently associated with significantly prolonged or heavy menstrual bleeding. The mechanism may be related to the increased total surface area as a result of the bulging uterine wall, impaired uterine wall contractility, or micro/macrovascular abnormalities.
- Features of mass effect
- Enlarged, firm and irregular uterus during bimanual pelvic examination
- Size can range from normal to full-term gestation
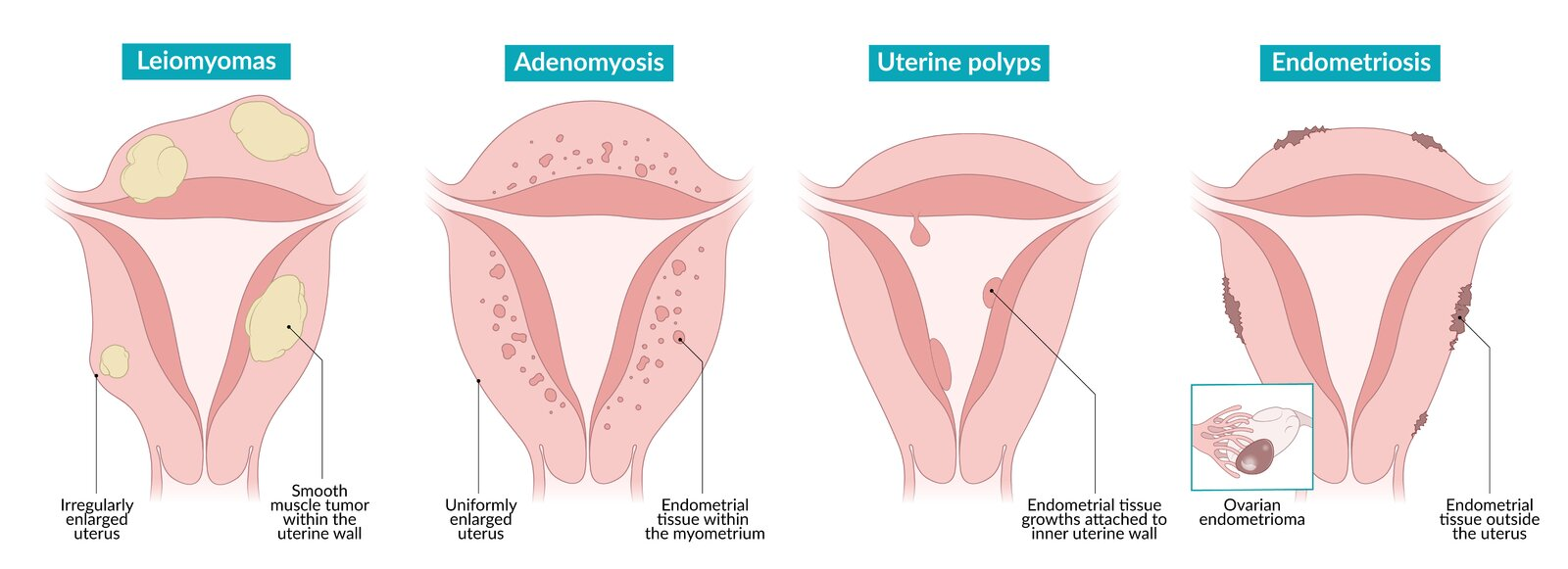
- Differ from Adenomyosis, which shows globular, uniformly enlarged uterus that is soft but tender on palpation
- Back or pelvic pain/discomfort
- Urinary tract or bowel symptoms (e.g., urinary frequency/retention/incontinence, constipation, features of hydronephrosis)
- Enlarged, firm and irregular uterus during bimanual pelvic examination
- Reproductive abnormalities
- Infertility (difficulty conceiving and increased risk of pregnancy loss)
- Related to an obstructed uterine cavity and/or impaired contractility of the uterus.
- Dyspareunia
- Infertility (difficulty conceiving and increased risk of pregnancy loss)
Diagnostics
Warning
Uterine leiomyomas are extremely common (affecting 70% of women) and are often found incidentally on ultrasound; do not attribute abnormal uterine bleeding to leiomyomas until other etiologies have been ruled out!
Pathology
- Macroscopic
- Grayish-white surface
- Homogeneous; tissue bundles on cross-section partly in a whorled pattern
- Some leiomyomas may involve regressive changes: scar formation, calcification, and cysts
- Microscopic: Smooth muscle tissue in a whorled pattern with well-demarcated borders, consisting of monoclonal cells interspersed with connective tissue
Differential diagnostics
Uterine leiomyosarcoma (uterine sarcoma)
Rare malignant tumor arising from the smooth muscle cells of the myometrium
- Risk factors
- Menopause
- Tamoxifen use
- Because it stimulate the ER on uterine myometrium
- Uterine findings
- Rapidly enlarging
- Pathology
- Single lesions with areas of coagulative necrosis and/or hemorrhage
- Cords of polygonal cells with eosinophilic cytoplasm, abundant mitoses, and cellular atypia are common.
Treatment
- Asymptomatic: Observation, as most fibroids shrink after menopause.
- Medical (symptom control):
- Hormonal contraceptives (e.g., OCPs) or progestin-releasing IUDs can manage heavy bleeding but do not shrink fibroids.
- GnRH agonists (e.g., leuprolide) induce a temporary menopause-like state, shrinking fibroids. Used short-term pre-operatively due to significant side effects.
- Surgical/Procedural:
- Myomectomy: Surgical removal of fibroids while preserving the uterus. This is the choice for patients who desire future fertility.
- Hysterectomy: Definitive treatment, removing the uterus and thus curing the fibroids.
- Uterine Artery Embolization (UAE): A minimally invasive procedure where embolic agents block blood flow to the fibroids, causing them to shrink.