Epidemiology
Etiology
Pathophysiology
- In endometriosis, endometrial tissue occurs outside of the uterus.
- It’s adenomyosis if in uterus.
- Common locations of endometriotic implants include:
- Pelvic organs
- Ovaries: most common site; often affected bilaterally
- Rectouterine pouch
- Fallopian tubes
- Bladder
- Cervix
- Peritoneum
- Extrapelvic organs (e.g., lung or diaphragm): less commonly affected
- Pelvic organs
- Regardless of where the endometrial tissue is located, it reacts to the hormone cycle in much the same way as the endometrium and proliferates under the influence of estrogen.
- Endometriotic implants result in:
- ↑ Production of inflammatory and pain mediators
- Anatomical changes (e.g., pelvic adhesions) → infertility
Clinical features
General
- Chronic pelvic pain that worsens before the onset of menses
- Infertility
- Endometriosis causes inflammation and adhesions that can change pelvic anatomy, altering egg quality and impairing implantation. 25–50% of infertile women have endometriosis.
- Dysmenorrhea
- Pre- or postmenstrual bleeding
- Dyspareunia
Intestines
- Dyschezia
- Diarrhea
- Constipation
- Rectal bleeding
Diagnostics
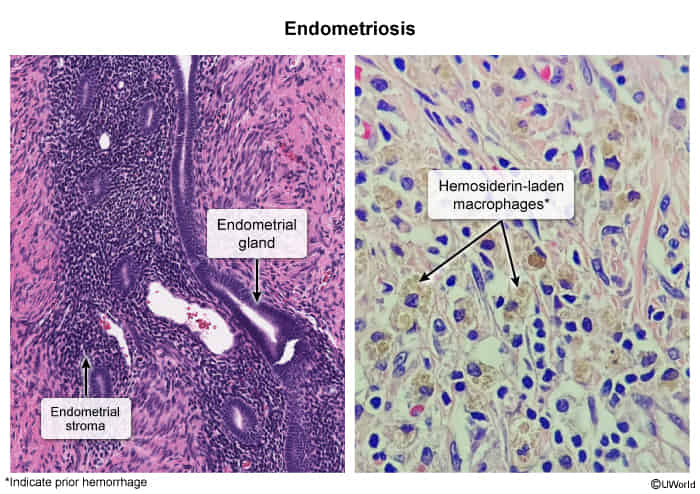
Pathology
- Normal endometrial glands
- Normal endometrial stroma
- Preponderance of hemosiderin laden macrophages due to cyclic hemorrhages into endometriomas
Differential diagnosis
Adenomyosis
Tip
- Endometriosis: fixed, immobile uterus (due to pelvic adhesion)
- Adenomyosis: enlarged, boggy, tender uterus
- Definition: benign disease characterized by the occurrence of endometrial tissue within the myometrium due to hyperplasia of the endometrial basal layer
- Epidemiology: peak incidence at 35–50 years
- Clinical features
- May be asymptomatic
- Dysmenorrhea
- Abnormal uterine bleeding
- Chronic pelvic pain, aggravated during menses
- Globular, uniformly enlarged uterus that is soft but tender on palpation
- Differ from Uterine leiomyoma, which shows irregularly enlarged, firm uterine
- Diagnostics
- Diagnosis is clinical and may be supported by transvaginal ultrasound and MRI findings
- Asymmetric myometrial wall thickening
- Myometrial cysts
- Diagnosis is clinical and may be supported by transvaginal ultrasound and MRI findings
Pathology
Macroscopic findings
- Ovaries
- Gunshot lesions or powder-burn lesions
- Black, yellow-brown, or bluish nodules or cystic structures
- Seen on the serosal surfaces of the ovaries and peritoneum
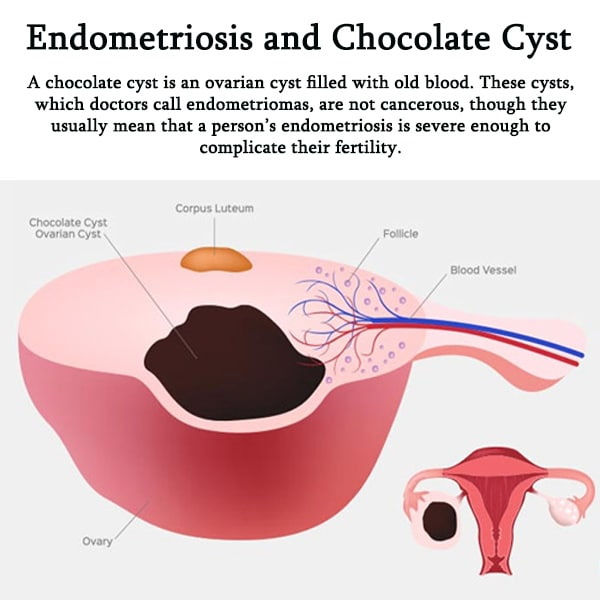
- Ovarian endometriomas or chocolate cysts: cyst-like structures that contain blood, fluid, and menstrual debris
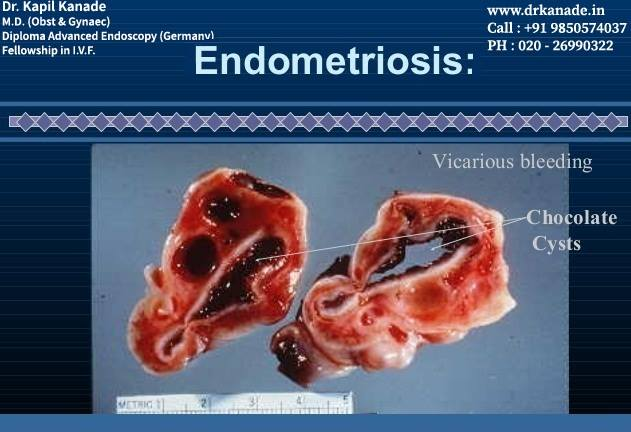
- Gunshot lesions or powder-burn lesions
Treatment
Endometriosis
- 1st Line (Pain): NSAIDs and combined oral contraceptives (OCPs).
- 2nd Line: Progestin-only therapies (e.g., medroxyprogesterone), GnRH agonists (e.g., Leuprolide) to induce a pseudomenopausal state.
- Surgical: Conservative laparoscopy for resection/ablation of implants (preserves fertility) or definitive surgery (TAH/BSO) for severe, refractory disease.
Adenomyosis
- Medical: Primarily aimed at symptom control (reducing bleeding/pain).
- Levonorgestrel-releasing IUD (Mirena) is highly effective.
- Combined OCPs or progestin-only therapy can also be used.
- Surgical:
- Hysterectomy is the only definitive treatment.
- Uterine artery embolization is an alternative for those wishing to avoid hysterectomy.