Etiology
Pathogens
- Escherichia coli: leading cause of UTI (approx. 80%)
- Ten times more common in females (shorter urethras colonized by fecal microbiota).
- Staphylococcus saprophyticus: 2nd leading cause of UTI in sexually active women
- Klebsiella pneumoniae: 3rd leading cause of UTI
- Proteus mirabilis
- Produces ammonia, giving the urine a pungent or irritating smell
- Associated with struvite stone formation
- Nosocomial bacteria: Serratia marcescens, Enterococci spp., and Pseudomonas aeruginosa are associated with increased drug resistance.
Tip
- Urethritis is often caused by sexually transmitted infections (STIs), e.g. N gonorrhoeae.
- UTIs are generally caused by bacteria from the gastrointestinal tract, e.g. E coli.
Classification
| Feature | Upper UTI (Pyelonephritis) | Lower UTI (Cystitis) |
|---|---|---|
| Location | Kidney / Renal Pelvis | Bladder / Urethra |
| Systemic Sx | Yes (Fever, Chills, Malaise) t | No (Typically Afebrile) |
| Key Sign | CVA Tenderness, Flank Pain | Suprapubic Tenderness |
| Urinary Sx | May be present | Predominant (Dysuria, Frequency) |
| UA KEY FINDING | WBC Casts | NO WBC Casts |
| Severity | More Severe | Less Severe |
| Management | Often Inpatient, IV Antibiotics | Usually Outpatient, Oral Antibiotics |
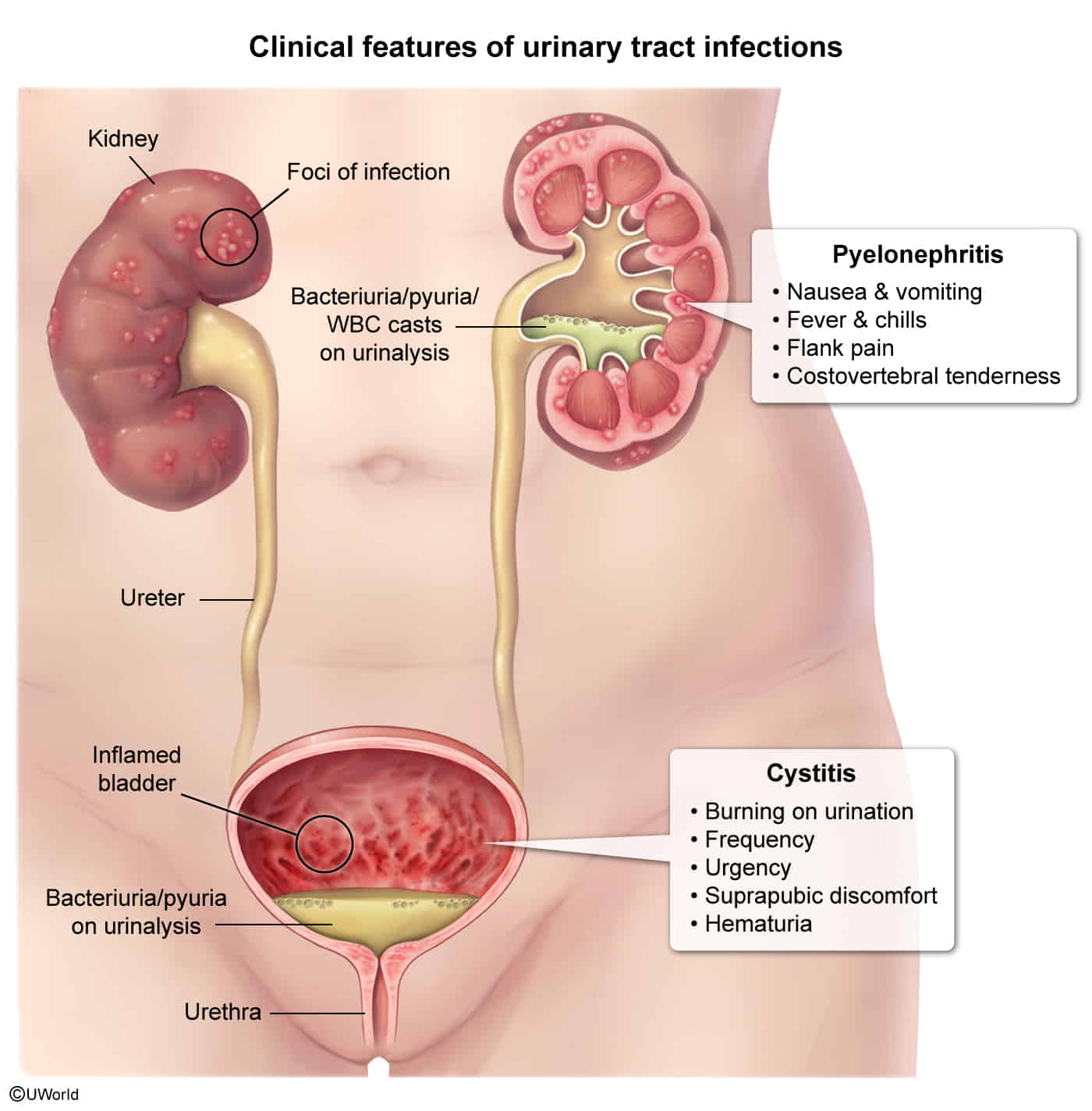 |
Clinical features
Diagnostics
Urinalysis
- Pyuria: presence of white blood cells (WBCs) in the urine
- Positive leukocyte esterase: an enzyme produced by WBC
- ≥ 5 WBC/HPF
- Bacteriuria: presence of bacteria in the urine
- Positive urinary nitrites: indicate bacteria that convert nitrates to nitrites (most commonly gram-negative bacteria; e.g., E.coli, Klebsiella, Proteus mirabilis)
- Other findings
- Leukocyte casts may indicate pyelonephritis.
- Micro- or macroscopic hematuria may be present.
- Alkaline urine (pH > 8) and struvite crystals in sediment: indicate urease-producing organisms (e.g., Proteus, Klebsiella, Staphylococcus saprophyticus)
Drawing 2025-03-29 16.01.03.excalidraw
⚠ Switch to EXCALIDRAW VIEW in the MORE OPTIONS menu of this document. ⚠ You can decompress Drawing data with the command palette: ‘Decompress current Excalidraw file’. For more info check in plugin settings under ‘Saving’
Excalidraw Data
Text Elements
Lactose Fermenters
Nitrate Reducers
Proteus
Urease Production
Helicobacter pylori Ureaplasma urealyticum Staphylococcus saprophyticus (3rd) Corynebacterium spp.
E. coli (1st) Enterobacter Citrobacter
Klebsiella (2nd)
Pseudomonas
Embedded Files
1d31e51a4dbefce0670aa7da4357fddf403fccdd: Gemini_Generated_Image_wapvdcwapvdcwapv.png
32b3a48d96d30b68f178804fbc510ef15c83cea3: Gemini_Generated_Image_ednoi4ednoi4edno.png
12d8036895fa186aba0d7b9b88f6b88c31682b83: Gemini_Generated_Image_o62ynao62ynao62y.png
Link to original
Treatment
- Uncomplicated Cystitis:
- First-line: Nitrofurantoin (5 days), TMP-SMX (3 days, if local resistance <20%), or Fosfomycin (single dose).
- Complicated Cystitis:
- Longer course (7-14 days) of oral fluoroquinolones (e.g., Ciprofloxacin) or TMP-SMX.
- Outpatient Pyelonephritis (Mild-to-Moderate):
- Oral fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin) for 7-14 days.
- Inpatient Pyelonephritis (Severe):
- IV antibiotics (e.g., Fluoroquinolones, extended-spectrum Cephalosporins like Ceftriaxone, or Piperacillin-tazobactam).
- Asymptomatic Bacteriuria:
- Generally not treated, except in pregnant patients or before urologic procedures.
Mnemonic
- 口诀——三光政策(急性膀胱炎治疗三天)首选喹诺酮类药物(妊娠的以及<18岁的首选三代头孢)
- 口诀——两个周瑜(急性肾盂肾炎治疗两周)喹诺酮类药物
UTI in pregnancy
- Pregnancy may increase the risk of recurrent bacteriuria and UTIs.
- Treatment
- Empiric antibiotics for ASB and lower UTI considered appropriate during pregnancy include:
- Fosfomycin
- Beta-lactam antibiotics for 5–7 days
- Oral cephalosporins (e.g., cefpodoxime)
- Aminopenicillins plus beta-lactamase inhibitors (e.g., amoxicillin/clavulanic acid)
- Empiric antibiotics for ASB and lower UTI considered appropriate during pregnancy include: