- Pathophysiology/Etiology
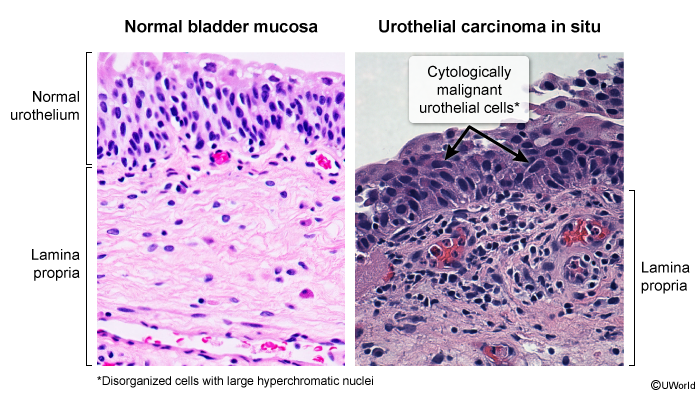
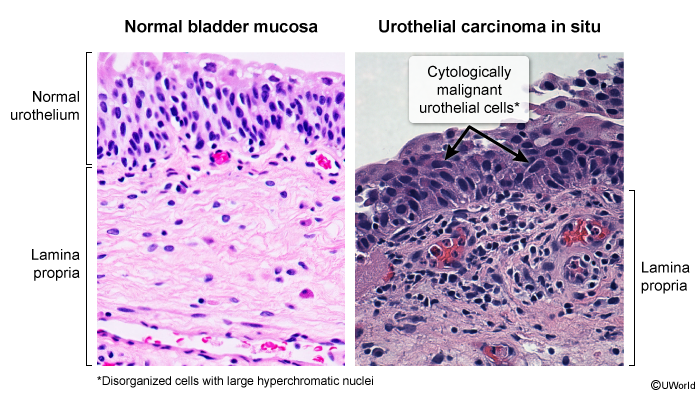
- Urothelial (Transitional Cell) Carcinoma (TCC): Most common type (~90%) in the US and Western world. Arises from the urothelium lining the bladder.
- Squamous Cell Carcinoma (SCC): Associated with chronic bladder irritation, such as from chronic infections, indwelling catheters, or Schistosoma haematobium infection (common in the Middle East/Africa).
- Adenocarcinoma: Rare type arising from mucus-secreting glands.
- Risk Factors (High Yield):
- Smoking: Most important risk factor; contains carcinogens like aromatic amines. t
- Occupational exposure: Chemicals used in textile, dye, rubber, and leather industries (e.g., aniline dyes, β-naphthylamine).
- Medications: Cyclophosphamide (chemotherapy agent).
- Chronic inflammation: Chronic UTIs, long-term catheter use.
- Age >55 and male sex.
- Clinical Presentation
- Painless gross hematuria: The classic and most common presenting symptom (in ~80-90% of patients). Any patient >40 years with painless hematuria should be evaluated for bladder cancer.
- Irritative voiding symptoms: Frequency, urgency, and dysuria can occur, especially with carcinoma in situ (CIS).
- Advanced disease: May present with pelvic pain, flank pain (from ureteral obstruction), or lower extremity edema.
- Diagnosis
- Cystoscopy with biopsy: Gold standard for diagnosis and initial staging. It allows direct visualization and tissue sampling to determine histology and depth of invasion.
- Urine Cytology: Can detect malignant cells in the urine, particularly useful for high-grade tumors and CIS.
- Urinalysis: Will show hematuria (microscopic or gross).
- Imaging (CT Urogram): Used to evaluate the entire urinary tract (kidneys, ureters, bladder) for tumors and to stage the cancer.
- DDx (Differential Diagnosis)
- Urinary Tract Infection (UTI): Usually presents with dysuria, frequency, and positive urine culture; hematuria can be present but often with other symptoms.
- Nephrolithiasis: Typically causes severe, colicky flank pain that may radiate to the groin, along with hematuria.
- Benign Prostatic Hyperplasia (BPH): Can cause irritative or obstructive voiding symptoms and hematuria.
- Renal Cell Carcinoma: Also presents with painless hematuria; imaging is key to differentiate.
- Management/Treatment
- Staging is crucial and divides cancer into non-muscle-invasive (NMIBC) and muscle-invasive (MIBC).
- Non-Muscle-Invasive (Ta, T1, CIS):
- Transurethral Resection of Bladder Tumor (TURBT): Primary procedure for both diagnosis and treatment of superficial tumors.
- Intravesical Therapy: Instillation of agents directly into the bladder post-TURBT to reduce recurrence. BCG (Bacillus Calmette-Guérin) is used for high-risk tumors; Mitomycin C is another option.
- Muscle-Invasive (≥T2):
- Radical Cystectomy: Standard treatment involving removal of the bladder, prostate/seminal vesicles (men), or uterus/ovaries/anterior vagina (women).
- Neoadjuvant Chemotherapy: Often given before radical cystectomy to shrink the tumor (e.g., cisplatin-based regimens).
- Chemoradiation: An alternative bladder-sparing option for select patients.
- Key Associations/Complications
- Multifocal Nature: TCC often has multiple tumors throughout the urothelium due to the “field effect” of carcinogens in urine.
- High Recurrence Rate: NMIBC has a high rate of recurrence, necessitating long-term surveillance with cystoscopy.
- Complications: Ureteral obstruction leading to hydronephrosis, metastatic disease (bone, lung, liver), and complications from treatment (e.g., urinary diversion issues after cystectomy).