Mechanism of Action
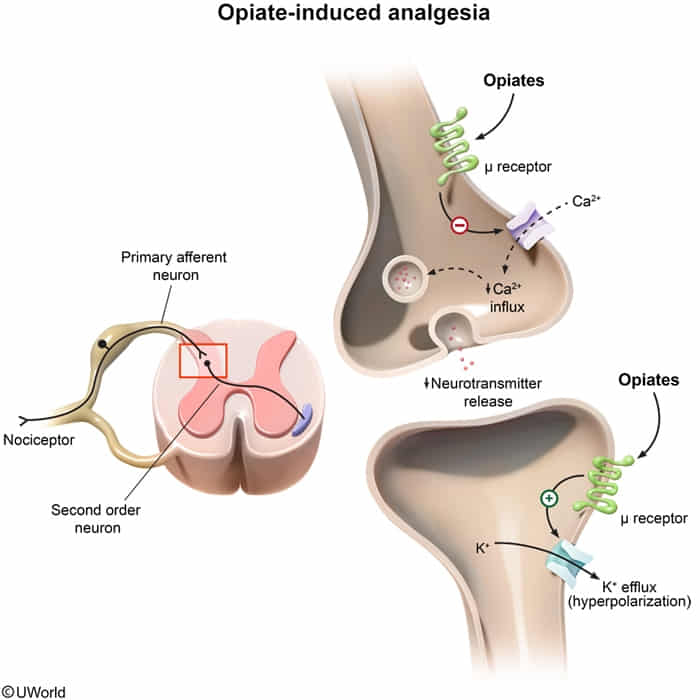
- Receptors: Act as agonists at opioid receptors (μ, δ, κ), which are Gi protein-coupled receptors. The μ-receptor is the most important for analgesia and the primary mediator of most clinical and adverse effects.
- Cellular Effect: Activation leads to closing of presynaptic voltage-gated Ca2+ channels (↓ neurotransmitter release, e.g., substance P, ACh, NE, glutamate) and opening of postsynaptic K+ channels (→ hyperpolarization, ↓ neuronal excitability).
- Overall Effect: Produces analgesia, sedation, and euphoria.
Classification
- Full agonists
- Morphine, heroin
- Methadone
- Meperidine
- Codeine
- Fentanyl
- Partial agonist: buprenorphine
- Mixed agonist/antagonists
- Butorphanol
- Nalbuphine
- Pentazocine
- Full antagonists
- Naloxone
- Naltrexone
- Methylnaltrexone
Strategies for safe opioid prescribing
- Optimize non-opioid interventions
- Use acetaminophen/NSAIDs, supportive care (eg, heat/ice) for mild/moderate pain
- Avoid routine opioid use for chronic pain
- Optimize opioid dose and duration
- Limit therapy to <5 days for acute pain
- Use lowest dose resulting in adequate pain control
- Avoid long-acting opioids
- Optimize monitoring
- Counsel patients on safe use; arrange close follow-up
- Educate patients on safe disposal of unused opioids
Adverse effects
- Constipation (not affected by tolerance, most common and persistent opioid side effect.)