Epidemiology
Etiology
- Arnold-chiari malformation, especially type I (most common cause)
- Posttraumatic Neuroloy physioloy injury (3–4% of patients with SCI develop symptomatic syringomyelia)
- Symptoms of syringomyelia may only develop months to years after the injury. The injury typically affects the cervical spine (e.g., following a motor vehicle accident).
Pathophysiology
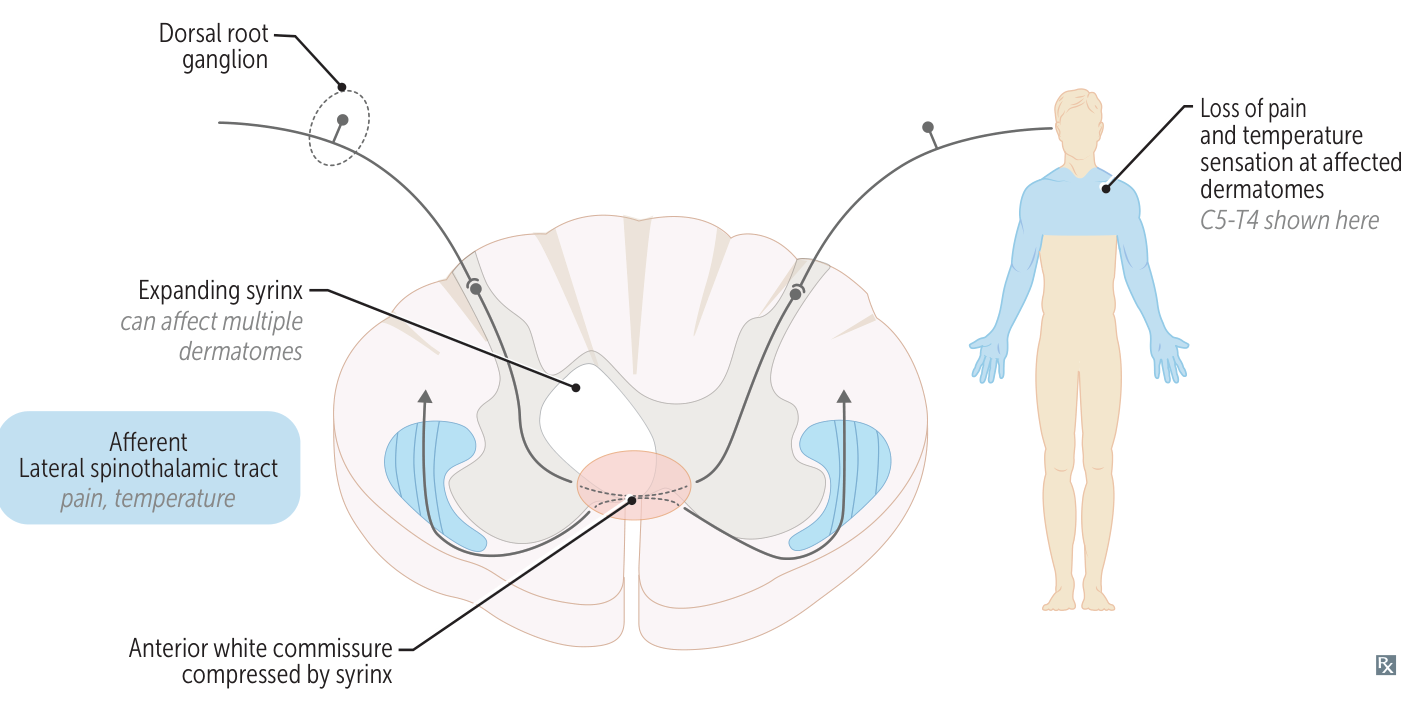
- Obstructed central canal of spinal cord (usually in the cervical spine, the thoracic or lumbar spine are less commonly affected) → impaired CSF drainage → formation of a dilated fluid-filled cavity in central spinal cord (syrinx)
- The syrinx expands and compresses adjacent structures.
- First structure damaged: Anterior White Commissure (contains decussating/crossing fibers of the spinothalamic tract).
- Late progression: Expansion may affect the anterior horn cells (LMN signs) and lateral corticospinal tract (UMN signs).
Tip
Syringomyelia is an abnormal fluid-filled dilation of the central canal of the spinal cord occurring as a result of impaired CSF flow.
Clinical features
- Often asymptomatic and/or slowly progressing (similar to central cord syndrome)
- Damages decussating fibers of the spinothalamic tract first.
- Classic presentation: Bilateral loss of pain and temperature sensation in a “cape-like” distribution (across the back, shoulders, and upper arms).
- Sensation of light touch, vibration, and proprioception (dorsal columns) is typically preserved early on.
- As the syrinx enlarges, it can affect:
- Anterior horns: LMN signs (weakness, atrophy, fasciculations) in the hands and arms.
- Lateral corticospinal tracts: UMN signs (spasticity, hyperreflexia) in the legs.
- Hypothalamospinal tract: Horner syndrome (ptosis, miosis, anhidrosis).