Epidemiology
Etiology
- Pathogen: Measles virus (Genus Morbillivirus, Family Paramyxoviridae).
- Structure: Enveloped, negative-sense, single-stranded RNA virus.
- Transmission: Respiratory droplets (highly contagious).
- Virulence factors:
- Hemagglutinin (H): Adhesion to host cells.
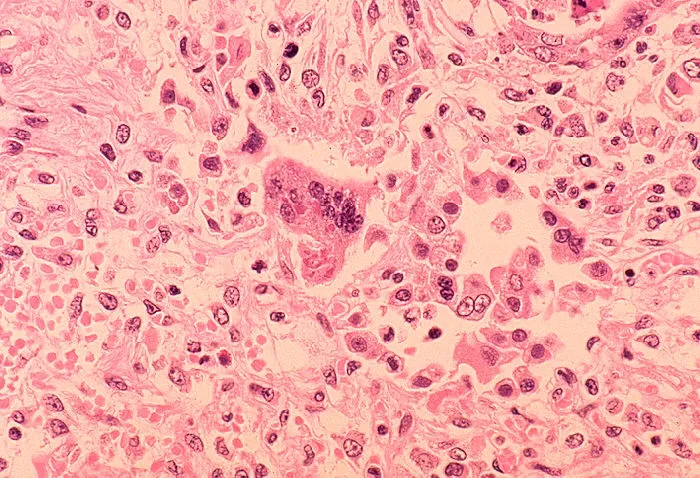
- Fusion (F) protein: Viral entry; causes formation of multinucleated giant cells (syncytia).
Pathophysiology
Clinical features
Mnemonic
烧三天、疹三天、退三天
- Prodrome (eg, cough, coryza, conjunctivitis, fever, Koplik spots)
- Maculopapular exanthem
- Cephalocaudal & centrifugal spread
- Spares palms & soles
Complications
Common Complications (Respiratory and GI)
- Pneumonia:
- This is the most common cause of measles-related death in children.
- Can be a secondary bacterial superinfection (e.g., S. pneumoniae, H. influenzae), which is most frequent.
- Can also be a primary viral pneumonia, known as Hecht’s giant cell pneumonia. This interstitial pneumonitis is characterized by multinucleated giant cells and is often seen in immunocompromised patients but can occur in healthy individuals and carries a high fatality rate.
- Otitis Media:
- An extremely common secondary bacterial infection, occurring in up to 1 in 10 children with measles. Can lead to hearing loss.
- Laryngotracheobronchitis (Croup):
- Inflammation of the upper airways can lead to the characteristic “barking” cough and stridor.
- Diarrhea:
- Frequently reported and can lead to significant dehydration, especially in young children.
Subacute sclerosing panencephalitis (SSPE)
- Etiology: Reactivation of defective Measles virus (mutated M protein); latency 7–10 years.
- Hx: Young patient with history of measles (or unvaxed) presenting with school failure and personality changes.
- Sx Progression: Behavioral regression → Myoclonus (jerking) → Dementia/Spasticity → Coma/Death.
- CSF: ↑↑ Anti-measles antibodies, oligoclonal bands.
- EEG: Periodic high-voltage slow waves.
- Histo: Demyelination + Intranuclear viral inclusions in neurons/oligodendrocytes.
- Tx: None (fatal).
Diagnostics
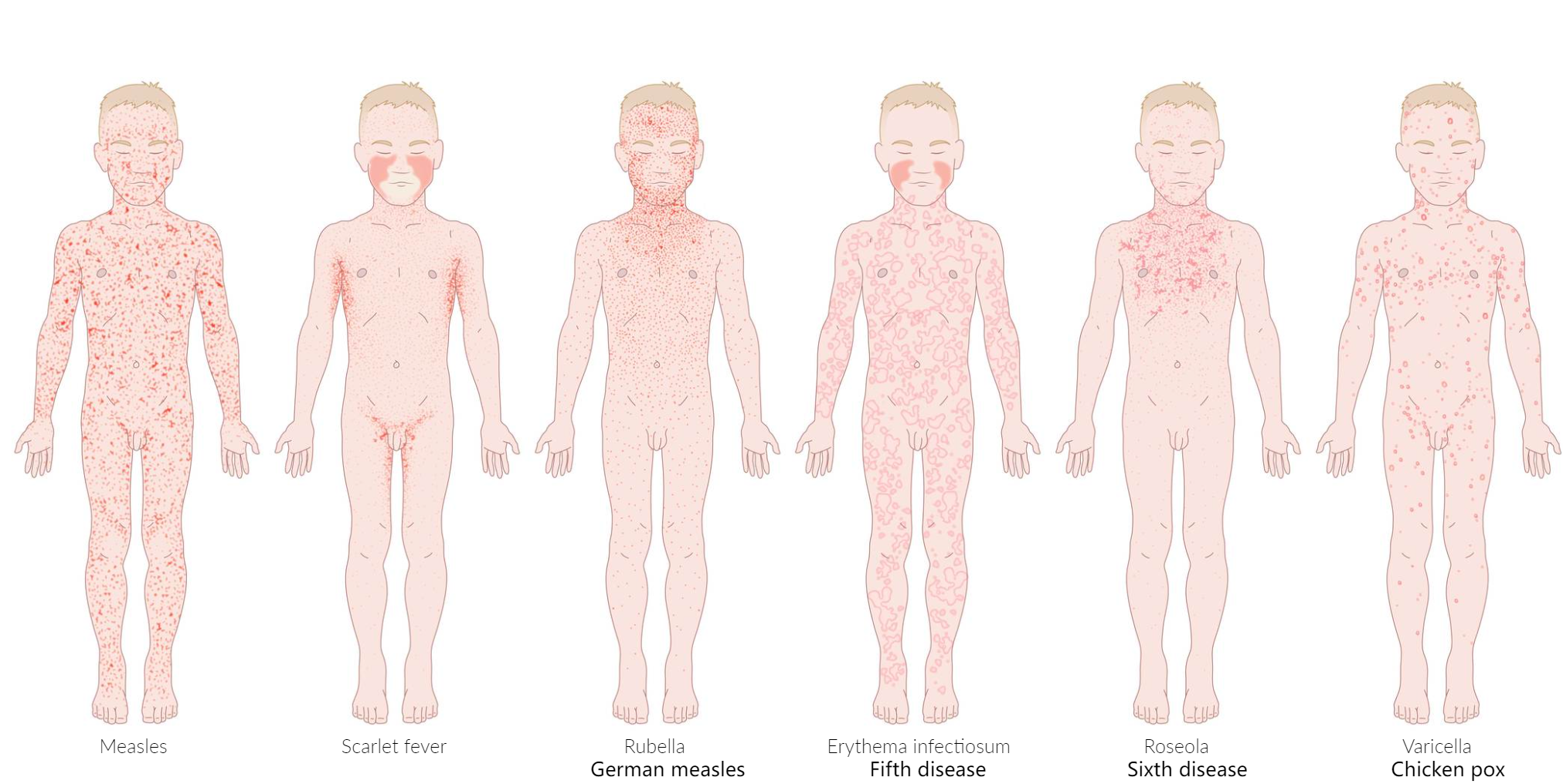
Childhood exanthems
Disease Pathogen Classic Presentation & Buzzwords Measles Measles virus 4 C’s (Cough, Coryza, Conjunctivitis, Koplik spots).
Rash: Face Body (Confluent).
Assoc: Vitamin A deficiency.Rubella Rubella virus Post-auricular LAD.
Rash: Face Body (spares 3 days, non-confluent).
Assoc: Congenital (PDA, cataracts, deaf), Adult arthritis.Roseola HHV-6 High fever breaks Rash appears.
Rash: Trunk Face.
Assoc: Febrile seizures.Fifth Disease Parvovirus B19 ”Slapped Cheek” Lacy/Reticular body rash.
Assoc: Aplastic crisis (Sickle Cell), Hydrops fetalis.Varicella VZV ”Dewdrop on a rose petal”.
Lesions in different stages of healing. t
Rash: Trunk Extremities.Scarlet Fever Strep pyogenes Sandpaper rash, Strawberry tongue, Circumoral pallor.
Assoc: Strep throat, Desquamation (palms/soles).
Fever-rash relationship
Link to original
- Measles (Rubeola): Fever first (with cough, coryza, conjunctivitis) → Rash appears 3-5 days later, spreading from head to toe.
- Rubella (German Measles): Low-grade fever → Rash appears 1-2 days later, spreading quickly from head to toe.
- Scarlet Fever: Fever and sore throat begin together → “Sandpaper” rash appears 1-2 days later.
- Erythema Infectiosum (Fifth): Low-grade fever/prodrome resolves → “Slapped cheek” rash appears days later.
- Roseola Infantum (Sixth): High fever for 3-5 days → Fever breaks → Rash appears after the fever is gone.
- Varicella (Chickenpox): Fever and vesicular rash appear at the same time (lesions in various stages).