Definition
- Dermatomyositis (DM): an inflammatory myopathy characterized by progressive symmetrical proximal muscle weakness and distinctive skin findings
- Polymyositis (PM): an inflammatory myopathy affecting the proximal skeletal muscles, with evidence of elevated CK and myositis on EMG and biopsy in the absence of any of the characteristic findings of the other IIM (a rare diagnosis of exclusion)
Epidemiology
Etiology
- Malignancy Association: strong association with occult malignancy (esp. adenocarcinomas of ovary, lung, pancreas, stomach) in Dermatomyositis. t
Pathophysiology
- Polymyositis:
- T-cell mediated cytotoxicity against skeletal muscle fibers.
- CD8+ T-cells infiltrate the endomysium (inner layer of muscle).
- Dermatomyositis:
- Humoral (antibody) and complement-mediated damage to microvasculature surrounding muscle.
- CD4+ T-cells infiltrate the perimysium (sheath around muscle fascicles).
Clinical features
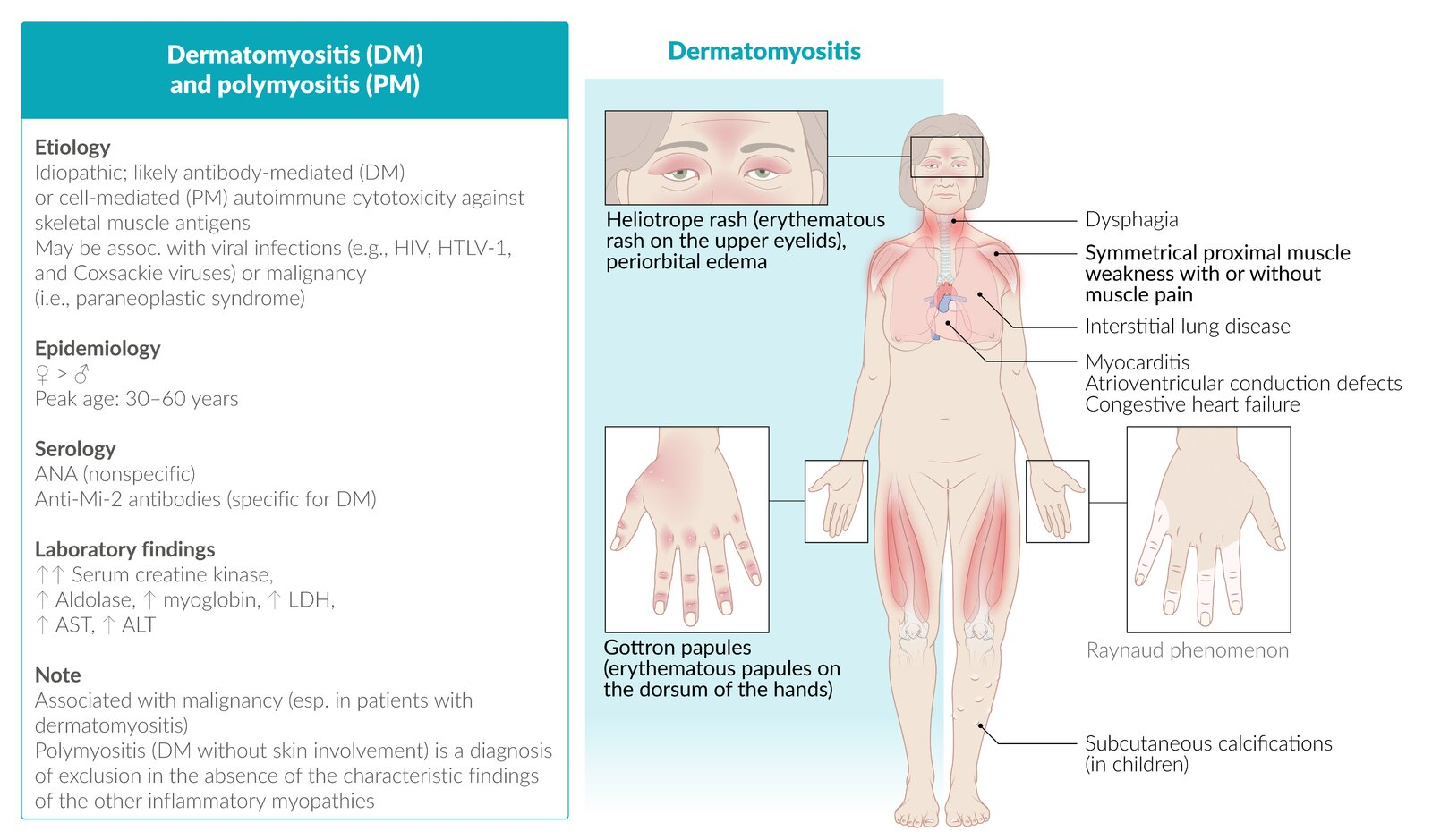
Muscle weakness
- Limb weakness
- Symmetrical proximal muscle weakness and atrophy
- Commonly affects pelvic and shoulder girdle muscles, leading to difficulties combing hair, standing up from a sitting position, and climbing stairs
- Axial muscle weakness
- Oropharyngeal muscle weakness leading to dysphagia
Cutaneous features
Cutaneous features are characteristic of dermatomyositis but may be found in other subtypes.
- Symmetric erythematous rash on the:
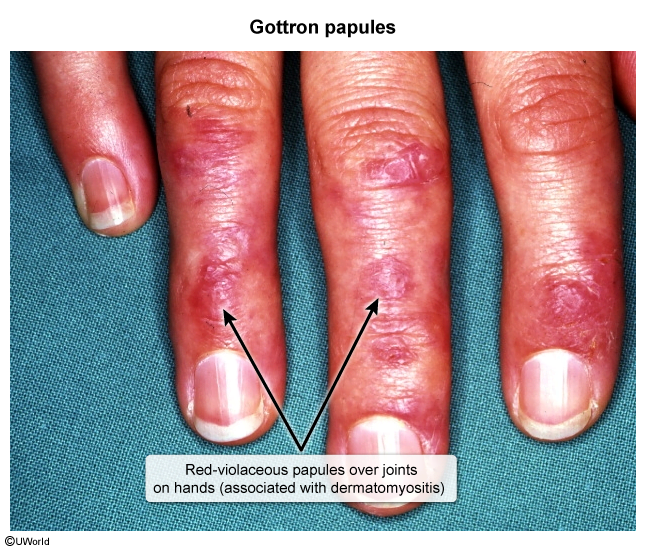
- Extensor surfaces of the hand joints, elbows, and knees (Gottron sign); scaly papules may form (Gottron papules)
- Upper eyelids (heliotrope rash); often associated with periorbital edema

- Mid-face
- Upper back, posterior neck, and shoulders (shawl sign)
- Upper chest and anterior neck (V sign)
- Extensor surfaces of the hand joints, elbows, and knees (Gottron sign); scaly papules may form (Gottron papules)
- Mechanic’s hands: thickened and cracked skin on the sides of the fingers and palms (horizontal fissures may appear darkened or dirty, hence the name)

Tip
The clinical features of PM is similar to DM except no cutaneous features.
Diagnostics
- ↑ CK
- Antinuclear antibodies (ANAs)
- Myositis-specific antibodies
- Anti-Jo-1 antibodies (anti–histidyl-tRNA synthetase)
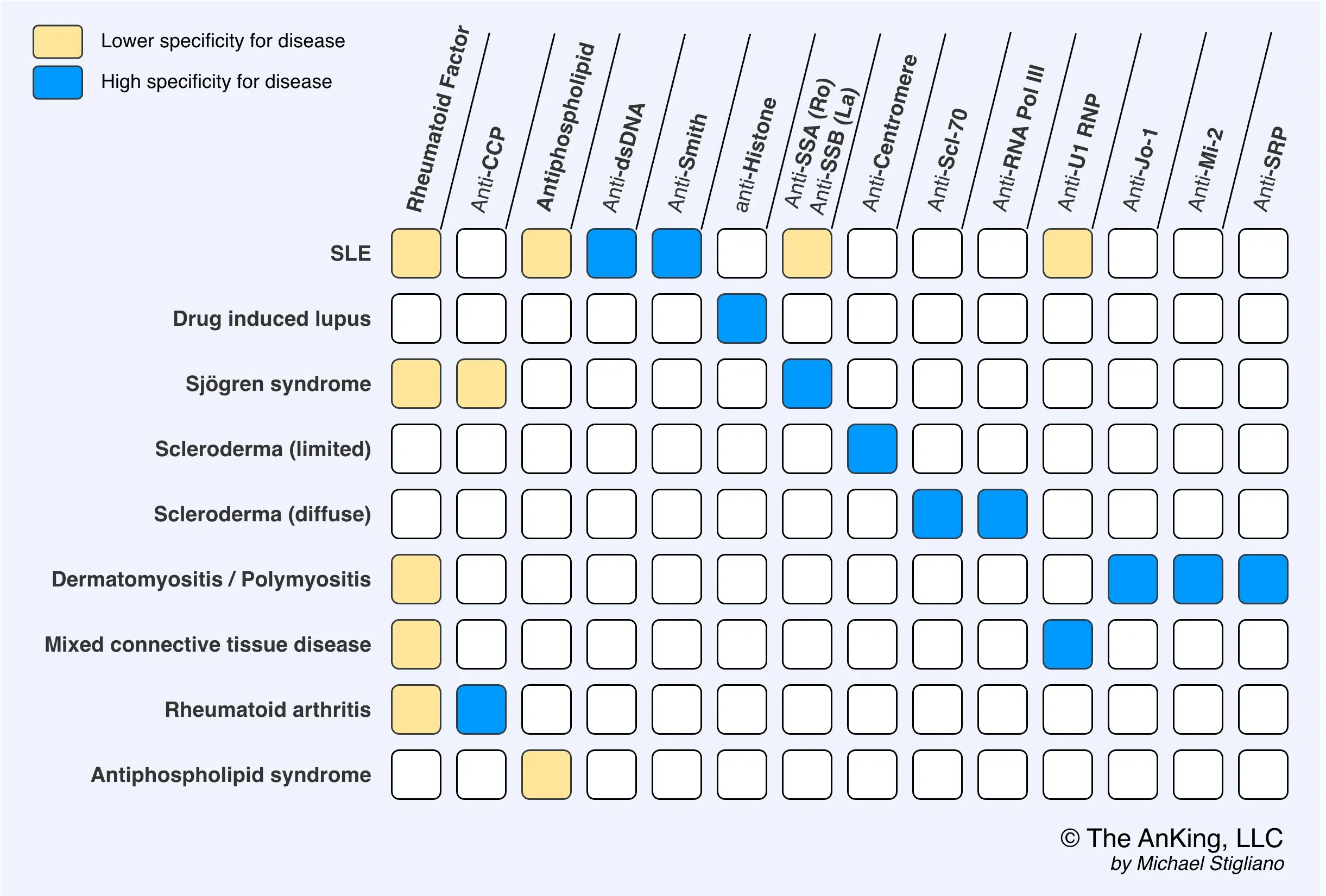
- Anti-Jo-1 antibodies (anti–histidyl-tRNA synthetase)
- Muscle biopsy: Gold standard for diagnosis of IIM
- Typical findings
- Muscle fiber damage
- Necrosis, degeneration, and regeneration
- Inflammatory cellular infiltrates
- DM: antibody-mediated inflammatory infiltrates that predominantly involve CD4+ T cells, plasmacytoid dendritic cells, and B lymphocytes in the perimysium (the connective tissue surrounding the fascicle); can lead to perifascicular atrophy
- IBM and PM: cell-mediated inflammatory infiltrates that predominantly involve cytotoxic CD8+ T cells in the endomysium (the connective tissue surrounding each muscle fiber), patchy necrosis
- Muscle fiber damage
- Typical findings
Differential diagnostics
Dermatomyositis vs. Systemic Sclerosis
| Feature | Dermatomyositis (DM) | Systemic Sclerosis (SSc) |
|---|---|---|
| Primary Issue | Muscle & skin inflammation (capillary damage) | Widespread fibrosis & vasculopathy |
| Key Skin | Gottron’s papules, Heliotrope rash, Shawl/V-sign, Mechanic’s hands | Skin thickening/tightening (scleroderma), Sclerodactyly, Telangiectasias, Calcinosis, Raynaud’s (often first) |
| Muscle | Symmetric proximal weakness (prominent), myalgias | Often mild or late; arthralgias/tendon rubs more common |
| Key Organ | Interstitial Lung Disease (ILD), dysphagia (skeletal muscle) | ILD, Pulmonary Arterial Hypertension (PAH), Esophageal dysmotility (smooth muscle), Scleroderma Renal Crisis |
| Antibodies | Anti-Jo-1 (ILD), Anti-Mi-2 (classic skin), Anti-MDA5 (amyopathic, severe ILD), Anti-TIF1-γ (cancer) | Anti-Scl-70 (diffuse, ILD), Anti-centromere (limited/CREST, PAH), Anti-RNA Pol III (renal crisis) |
| Malignancy | High risk (ovary, lung, etc.) | Slight increase (e.g., lung with ILD) |
| Tx Pearl | Corticosteroids, immunosuppressants; Cancer screening crucial | Organ-based; ACE Inhibitors for Renal Crisis (VITAL!) |
| Subtype/Note | Amyopathic DM (skin, no weakness) | Limited (CREST) vs. Diffuse variants |