Epidemiology
- Onset of symptoms usually occurs at 3–6 months of age.
- Disease often improves with age.
Etiology
Pathophysiology
- Multifactorial, involving genetic predisposition, immune dysregulation, and environmental factors leading to a defective epidermal barrier.
- Key genetic factor: Loss-of-function mutations in the filaggrin (FLG) gene are present in up to 30% of patients, impairing skin barrier function and moisture retention.
- Immune dysregulation: Characterized by a Th2-dominant inflammatory response, leading to increased IgE production and eosinophilia.
- Barrier dysfunction: A compromised stratum corneum leads to increased transepidermal water loss (TEWL), resulting in dry, itchy skin (xerosis) that is more susceptible to irritants and allergens.
Clinical features
Tip
- The symptoms of atopic dermatitis are variable and often change in the course of a lifetime. Pruritus and dry skin are usually the main symptoms.
- Most patients have a history of other atopic disorders
- Flares with low humidity (eg, winter months) or excessive heat
- Main symptoms: intense pruritus and dry skin
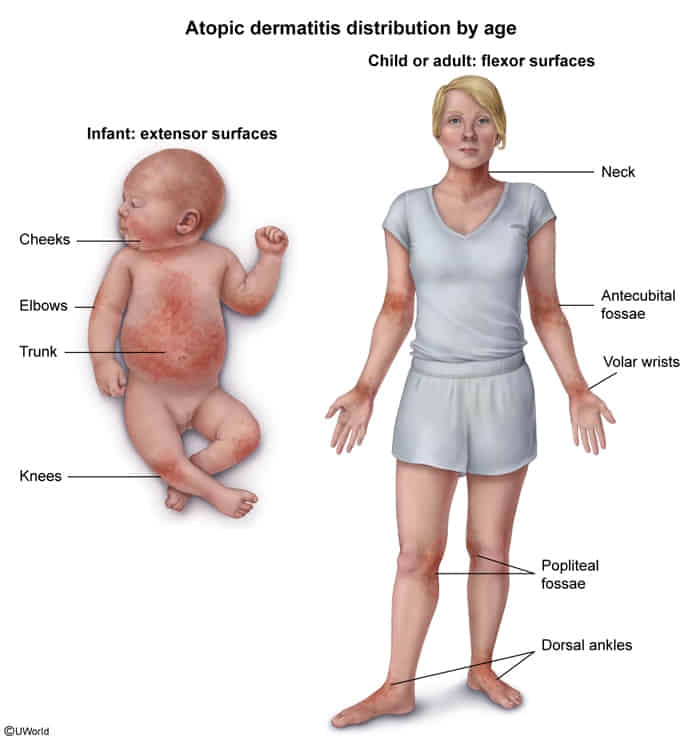
- Infantile AD (age < 2 years)
- Eczema involving the face, head, and extensor surfaces of the extremities that usually spares the diaper area
- May present initially with features similar to seborrheic dermatitis, e.g., cradle cap
- Dennie-Morgan fold: increased folds below the eye
- as a result of eyelid dermatitis

- as a result of eyelid dermatitis
- Occasionally, lesions appear on the trunk.
- Childhood AD (age 2–12 years)
- Eczema: flexural creases (antecubital fossa and popliteal fossa), skin folds, extensor surface of hands

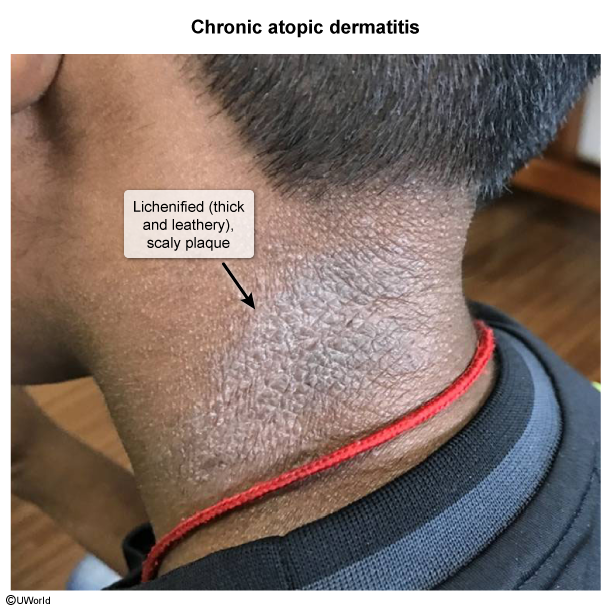
- Lesions usually become lichenified (thickening of the skin with accentuated skin markings).
- Eczema: flexural creases (antecubital fossa and popliteal fossa), skin folds, extensor surface of hands
- Adult/adolescent AD (age > 12 years)
- Lichenified lesions and pruritus of flexor surfaces of the extremities
- Antecubital fossae are frequently involved.
- Adult AD may also present as nummular eczema.
- Associated skin findings in AD
- Atopic triad: a triad of asthma, allergic rhinitis, and atopic dermatitis that is linked to allergen-triggered IgE-mast cell activation
- Food allergies
- Keratosis pilaris: keratinized hair follicles (rough bumps) typically distributed over extensor arms and thighs
- Hertoghe sign: thinning or loss of the outer third of the eyebrows
Diagnostics
- Atopy
- Personal and/or family history
- Immunoglobulin E reactivity (↑ serum IgE)
- Comorbid atopic diseases (i.e., asthma, allergic rhinitis, allergic conjunctivitis, and food allergies)
- Pathology
- Acute Eczema:
- Spongiosis: Epidermal intercellular edema (fluid accumulation between keratinocytes), which separates cells and makes “spines” (desmosomes) prominent.
- Intraepidermal vesicles.
- Chronic Eczema: Driven by the “Itch-Scratch Cycle”.
- Acanthosis: Diffuse epidermal hyperplasia (thickening of the stratum spinosum).
- Hyperkeratosis: Thickening of the stratum corneum.
- Parakeratosis: Retention of nuclei in the stratum corneum.
- Dermis: Perivascular lymphocytic infiltrate with eosinophils.
- Acute Eczema:
Treatment
- Maintenance: Emollients (restore barrier), avoid triggers.
- First-Line: Topical Corticosteroids.
- Low potency (face/folds); Medium-High potency (body).
- Second-Line (or Face/Eyelids): Topical Calcineurin Inhibitors (Tacrolimus).
- Key USMLE pt: No skin atrophy (unlike steroids).
- Severe/Refractory: Dupilumab (blocks IL-4/IL-13), Phototherapy, JAK inhibitors.
- Complications: Eczema Herpeticum (HSV superinfection) → Acyclovir.