Epidemiology
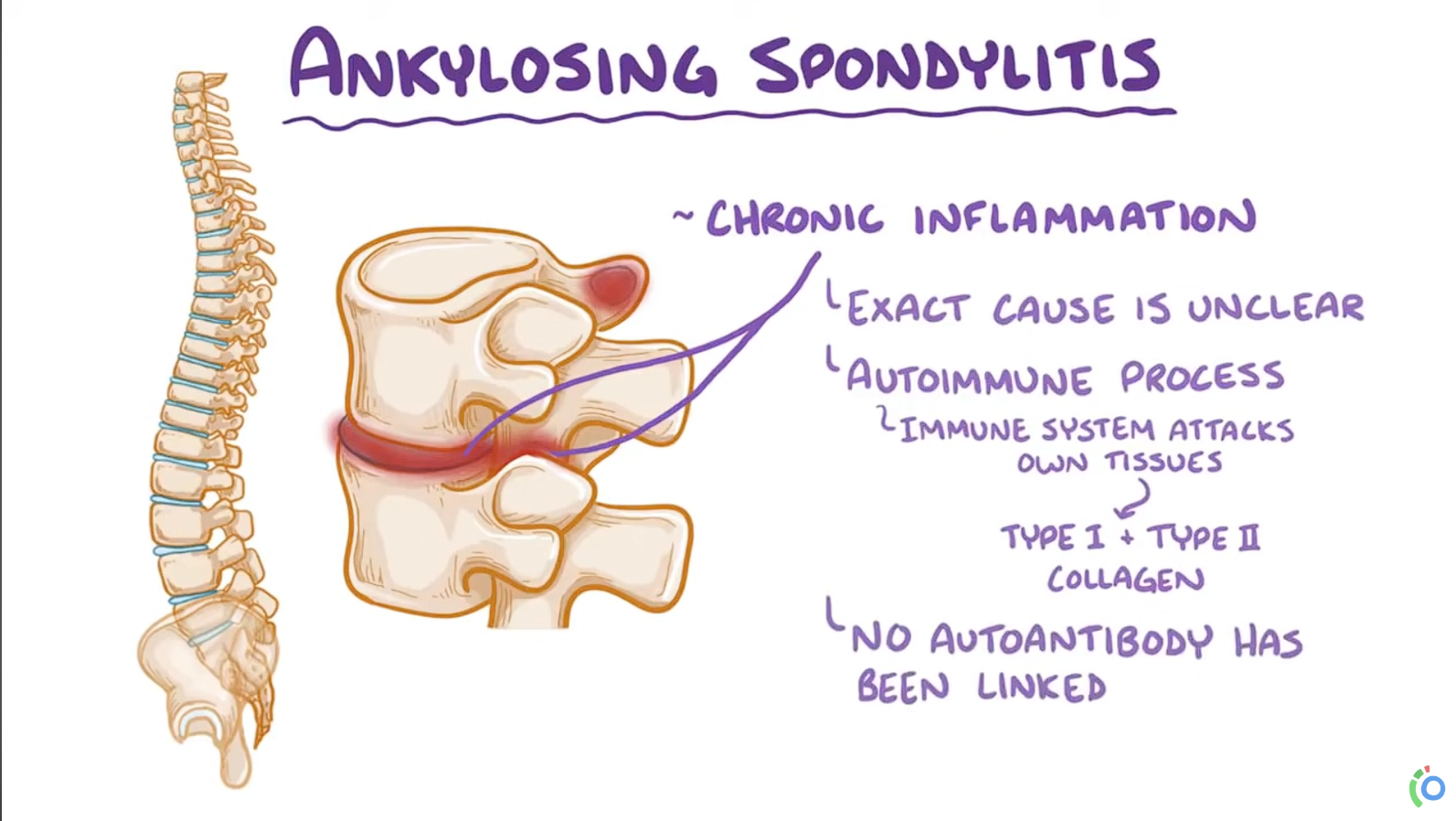
Etiology
- Genetic predisposition: 90–95% of patients are HLA-B27 positive.
Pathophysiology
- AS is distinct from rheumatoid arthritis:
- AS → simultaneous bone erosion AND new bone formation.
- Rheumatoid arthritis → primarily only erosions.
- Genetic/Immune Trigger: AS is strongly linked to HLA-B27. It is believed that in genetically susceptible individuals, factors like biomechanical stress or gut microbes trigger an immune response. This process activates the IL-23/IL-17 pathway, which is central to the disease. Misfolding of the HLA-B27 protein may also induce a cellular stress response that promotes IL-23 production.
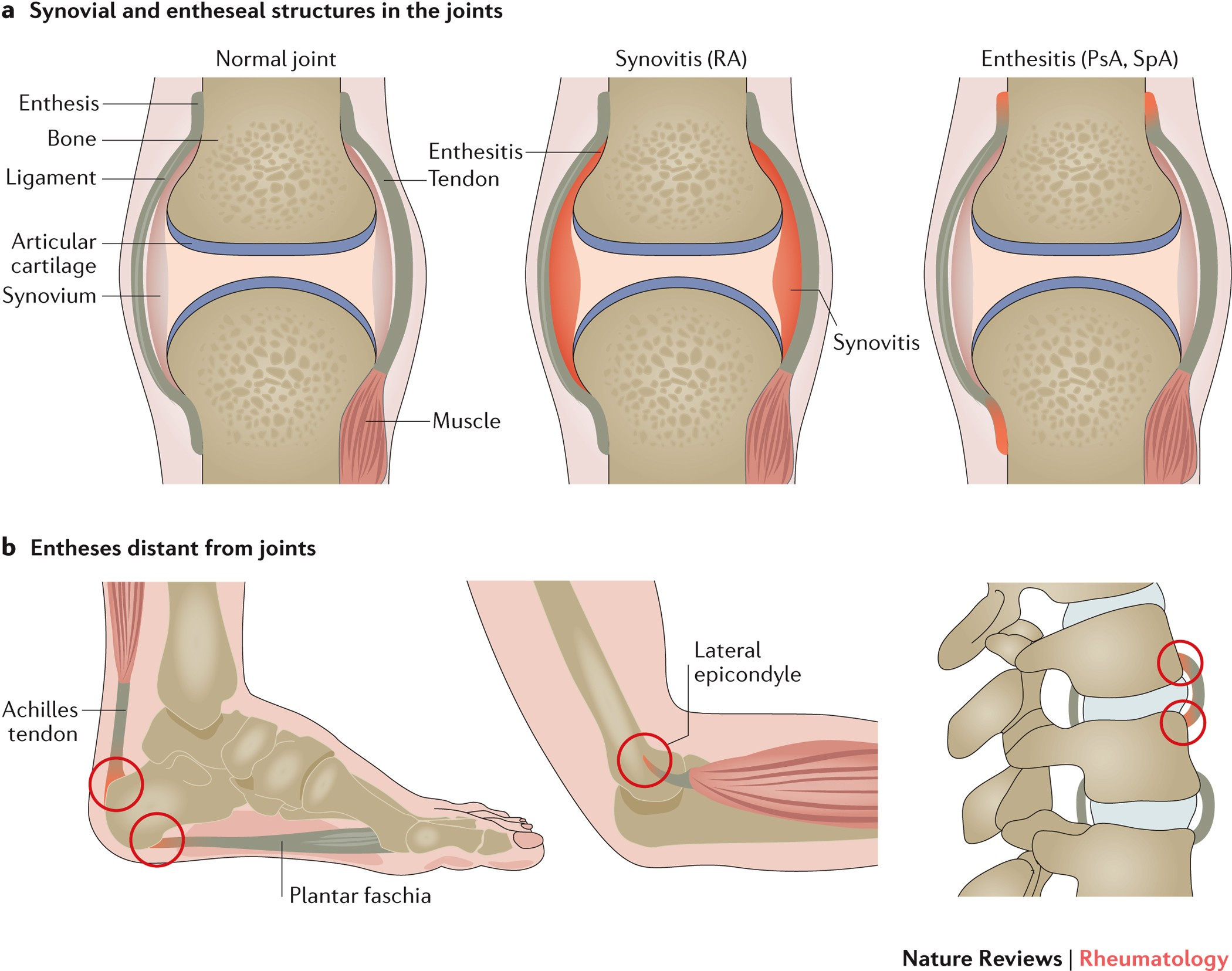
- Enthesitis (Core Pathology): The primary site of inflammation is the enthesis, where ligaments and tendons attach to bone. Cytokines like TNF-α and IL-17 drive this intense inflammation at the entheses.
- Pathologic Bone Formation: Chronic inflammation leads to erosion followed by abnormal healing. This results in pathologic new bone formation (syndesmophytes) and calcification of spinal ligaments. Over time, this process causes fusion of the sacroiliac joints and vertebrae, leading to the characteristic “bamboo spine” and spinal rigidity.
Clinical features
- Inflammatory back pain (sacroiliitis)
- Insidious onset at age <40
- Morning stiffness > 30 minutes that improves with activity
- Pain is independent of positioning
- Relieved with exercise, worse with rest (overnight & in the morning)
- Relieved with activity & warm showers
- Nocturnal pain
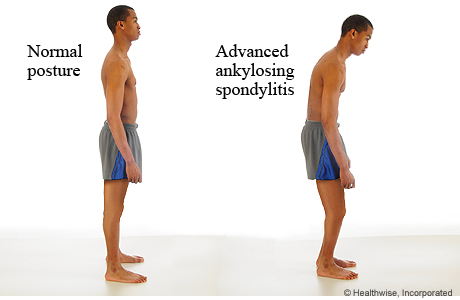
- Reduced chest expansion & spinal mobility
- Stiff or stooped posture
- Tenderness at spine, sacroiliac joints & peripheral tendon insertions (eg, Achilles)
- Enthesitis (tenderness at tendon insertion sites)
- Dactylitis (swelling of fingers & toes)
- Uveitis
Diagnostics
AS is a seronegative spondyloarthropathy, and there are no serologic tests to confirm the diagnosis.
Laboratory findings
- Elevated ESR & CRP
- HLA-B27: Positive in 90–95% of patients with axial spondyloarthritis
- Autoantibodies (e.g., rheumatoid factor, antinuclear antibodies) are negative
X-ray
- Sacroiliitis: bone erosions, subchondral sclerosis, eventual bony fusion (ankylosis)
- Bridging syndesmophytes: ossification at vertebral body margins (bamboo spine)
Treatment
- Cornerstone Tx:
- Physical therapy & exercise to maintain posture and flexibility.
- NSAIDs (e.g., Naproxen) are the first-line drug therapy.
- Second-Line Tx (if NSAIDs fail):
- TNF-α inhibitors (e.g., Adalimumab, Infliximab) are the best for axial symptoms.
- IL-17 inhibitors (e.g., Secukinumab) are an alternative.
- Specific Manifestations:
- Peripheral Arthritis: Sulfasalazine may be effective.
- Acute Anterior Uveitis: Treat with topical corticosteroids. Use TNF-α monoclonal antibodies (Infliximab/Adalimumab) for prevention in recurrent cases.
- Agents with Limited Efficacy for Axial Disease:
- Methotrexate & systemic glucocorticoids are generally not effective for spine/SI joint inflammation.