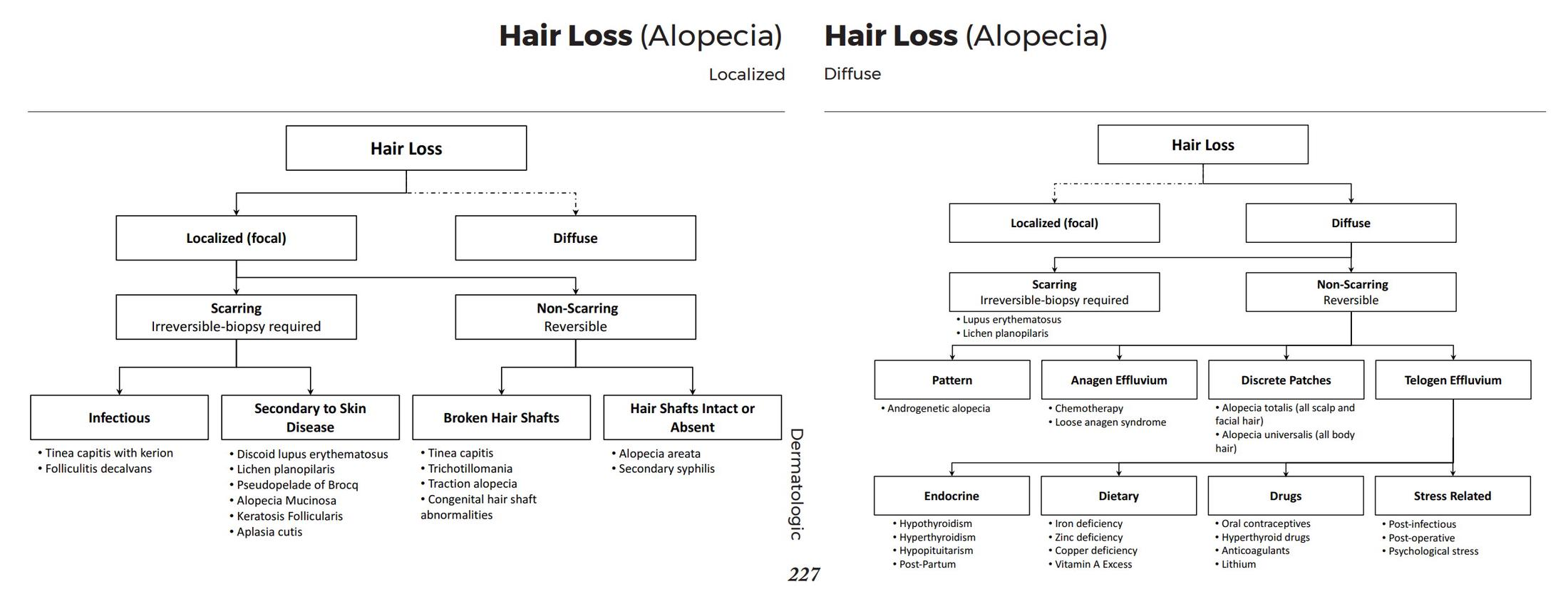
Alopecia, or hair loss, is broadly categorized into non-scarring (non-cicatricial) and scarring (cicatricial) types. Non-scarring alopecias have preserved hair follicles and are potentially reversible, while scarring alopecias involve irreversible destruction of hair follicles replaced by fibrous tissue.
Non-Scarring Alopecia
In these conditions, the hair follicle is not permanently damaged.
- Androgenetic Alopecia
- Etiology/Pathophysiology: This is the most common cause of hair loss. It is a genetically predetermined response to androgens (specifically dihydrotestosterone, or DHT). DHT leads to the progressive miniaturization of terminal hair follicles into vellus hairs. The condition is polygenic with variable expressivity.
- Clinical Features: It presents with a gradual onset of patterned hair thinning. In males, this typically involves bitemporal recession and thinning at the vertex. In females, it manifests as diffuse thinning over the crown with a wider central part, often sparing the frontal hairline.
- Treatment:
- Minoxidil: A topical vasodilator.
- Finasteride: An oral 5α-reductase inhibitor that prevents the conversion of testosterone to DHT.
- Spironolactone: An anti-androgen used for female-pattern hair loss.
- Telogen Effluvium
- Etiology/Pathophysiology: This condition occurs due to a premature shift of a large number of hairs into the telogen (shedding) phase. It is typically triggered by a significant physiological or psychological stressor 2-3 months prior to the hair loss. Common triggers include childbirth, high fever, major surgery, severe emotional stress, and certain medications.
- Clinical Features: Patients report acute, diffuse hair shedding all over the scalp.
- Diagnostics: A gentle “hair pull test” will yield numerous hairs.
- Treatment: The condition is usually self-limiting, with hair regrowth occurring once the underlying stressor is removed.
- Alopecia Areata
- Etiology/Pathophysiology: This is an autoimmune disorder where T-lymphocytes attack the hair follicles, leading to a loss of their “immune privilege.”
- Clinical Features: It classically presents as round or oval, well-demarcated, smooth patches of non-scarring hair loss. Other presentations include alopecia totalis (complete scalp hair loss) and alopecia universalis (complete body hair loss). Nail pitting can also be seen.
- Treatment:
- Corticosteroids: Can be administered topically, as intralesional injections, or orally.
- Topical Immunotherapy: Involves agents like diphencyprone.
- JAK inhibitors: Such as baricitinib, are newer targeted therapies for severe cases.
- Tinea Capitis
- Etiology/Pathophysiology: This is a dermatophyte (fungal) infection of the scalp, most commonly seen in children. Trichophyton tonsurans is a frequent cause in the United States.
- Clinical Features: It can present as scaly patches with hair loss, often with characteristic “black dots” from broken hair shafts. It may be accompanied by posterior cervical lymphadenopathy. An intensely inflammatory form called a kerion can also occur.
- Diagnostics: A KOH prep of plucked hairs can reveal fungal elements. A Wood’s lamp examination may cause some species, like Microsporum, to fluoresce.
- Treatment: Requires oral antifungal therapy, as topical treatments are insufficient. Options include griseofulvin and terbinafine.
Scarring Alopecia
These conditions involve inflammation that leads to permanent destruction of hair follicles.
- Discoid Lupus Erythematosus (DLE)
- Etiology/Pathophysiology: DLE is a chronic form of cutaneous lupus erythematosus. It is an autoimmune condition characterized by inflammation that damages the skin and hair follicles.
- Clinical Features: Patients develop well-demarcated, scaly, erythematous plaques that progress to atrophic, scarred patches with permanent hair loss. These lesions often show both hyper- and hypopigmentation and follicular plugging. The “carpet tack” sign, where adherent scales show spiky undersurfaces, can be seen.
- Treatment: Potent topical or intralesional corticosteroids and antimalarials like hydroxychloroquine are used to control inflammation and prevent further scarring.
- Lichen Planopilaris (LPP)
- Etiology/Pathophysiology: This is a form of lichen planus that specifically targets hair follicles, causing a lymphocytic inflammatory response that leads to their destruction.
- Clinical Features: It is characterized by perifollicular erythema and scaling around the hairs at the edges of active alopecic patches. The scalp within the patches appears smooth and white due to the loss of follicular openings. Patients often report itching, burning, or tenderness. Frontal fibrosing alopecia is considered a variant of LPP.
- Treatment: The goal is to halt progression with anti-inflammatory agents like corticosteroids, hydroxychloroquine, or tetracyclines.