Left part is for HIV, right part is for other virus.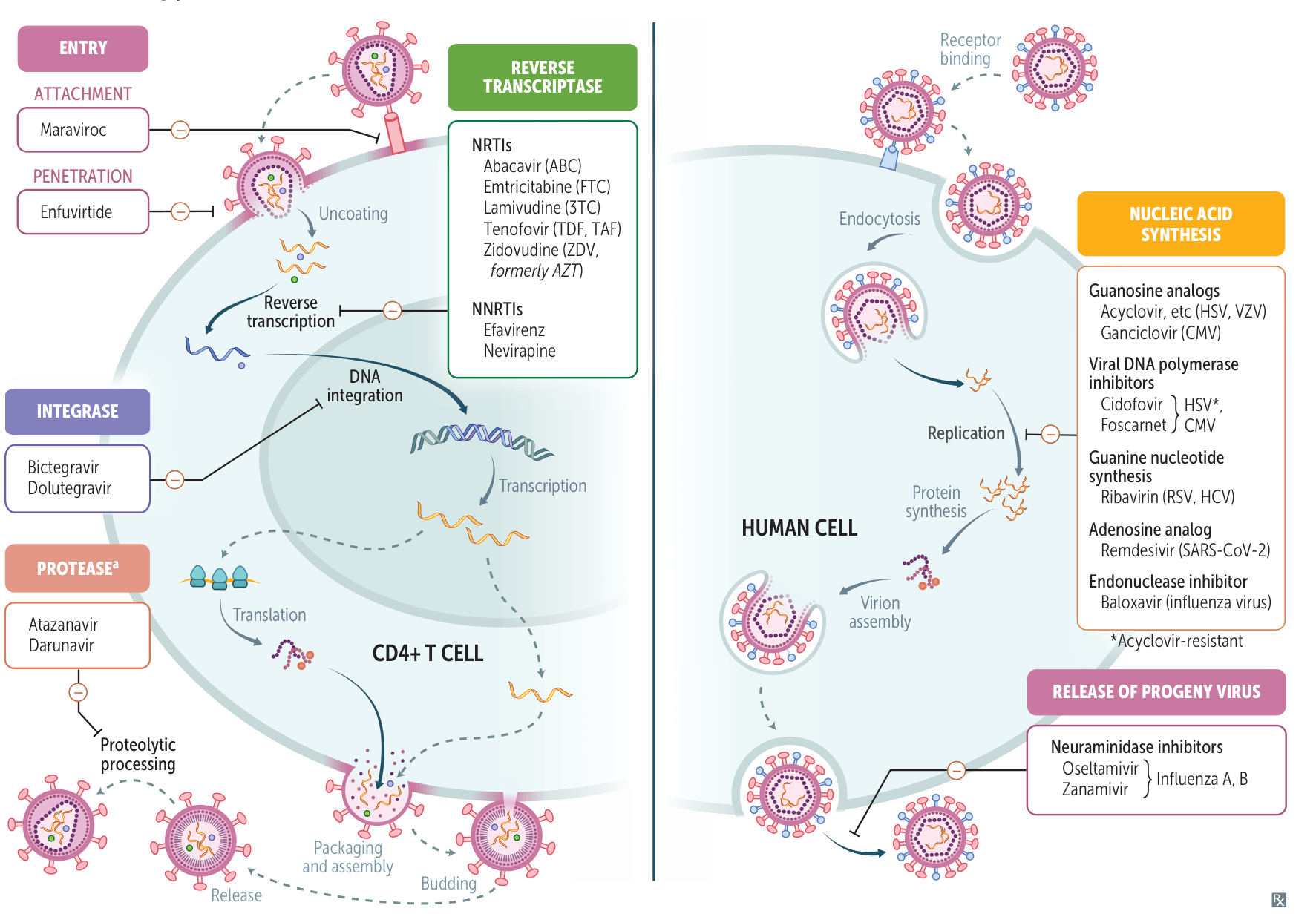
Tip
See HIV therapy for NRTIs and NNRTIs…
Anti-herpesvirus Agents
- Acyclovir, Valacyclovir, Famciclovir
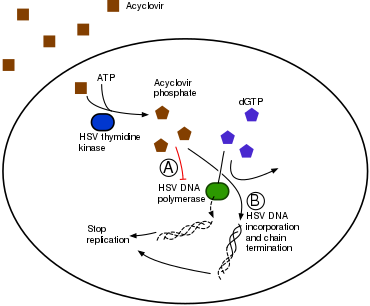
- Mechanism: Guanosine analogs. Require phosphorylation by viral thymidine kinase (TK) for activation → inhibit viral DNA polymerase → chain termination. Valacyclovir (prodrug of acyclovir) and famciclovir have better oral bioavailability.
- Clinical Use: HSV-1, HSV-2, VZV. Ineffective against CMV and EBV due to different or minimal TK activity.
- Adverse Effects: Obstructive crystalline nephropathy, neurotoxicity (confusion, hallucinations). Preventable with adequate hydration. t
- Resistance: Mutated viral TK.
- Ganciclovir, Valganciclovir
- Mechanism: Guanosine analog. Requires phosphorylation by CMV-specific protein kinase UL97 for activation → inhibits viral DNA polymerase.
- Clinical Use: CMV, especially retinitis in immunocompromised patients.
- Adverse Effects: Bone marrow suppression (leukopenia, neutropenia, thrombocytopenia), nephrotoxicity.
- Foscarnet
- Mechanism: Pyrophosphate analog. Directly inhibits viral DNA/RNA polymerase and HIV reverse transcriptase without requiring kinase activation.
- Clinical Use: CMV retinitis in immunocompromised patients; acyclovir-resistant HSV/VZV.
- Adverse Effects: Nephrotoxicity, electrolyte abnormalities (hypo/hypercalcemia, hypo/hyperphosphatemia, hypokalemia, hypomagnesemia) → can cause seizures.
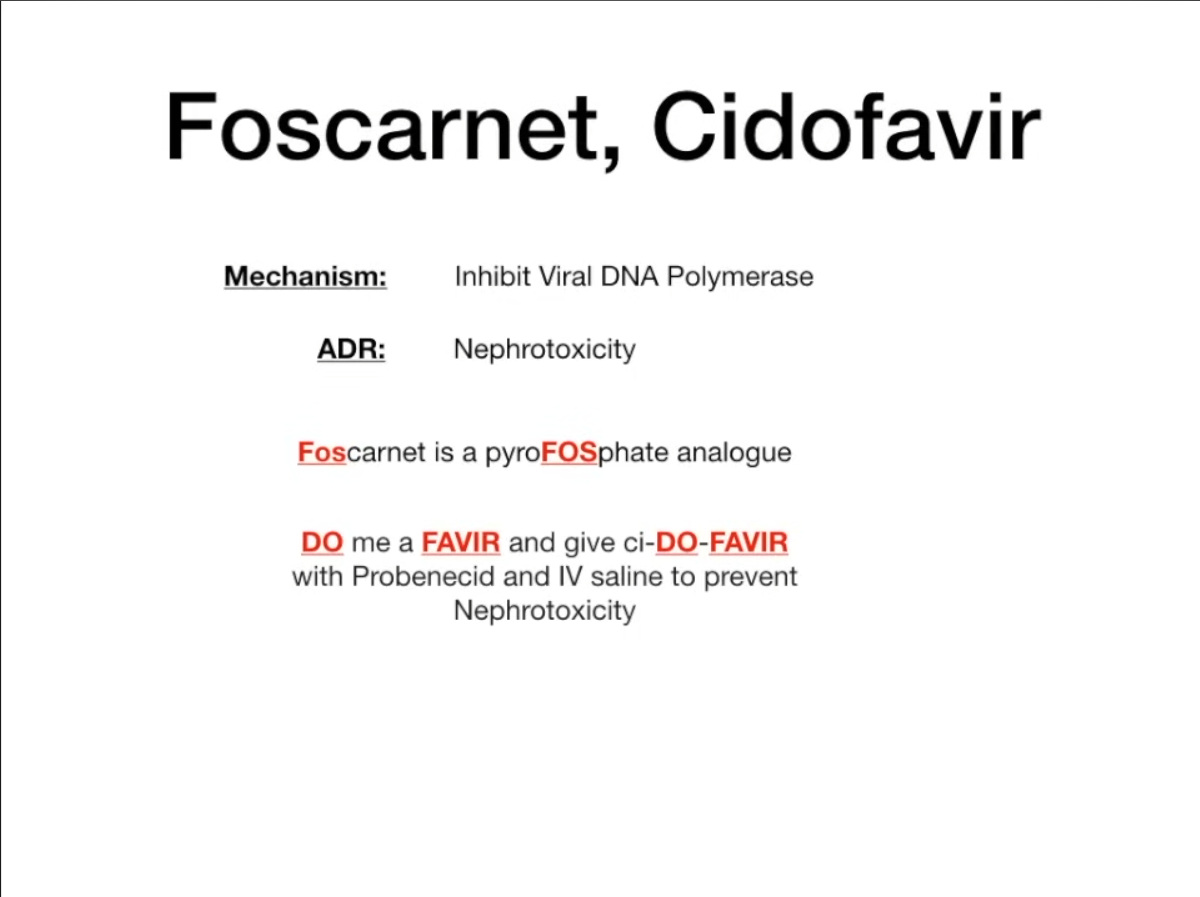
- Cidofovir
- Mechanism: Cytosine nucleotide analog. Directly inhibits viral DNA polymerase, does not require viral kinase activation.
- Clinical Use: CMV retinitis in HIV patients.
- Adverse Effects: Nephrotoxicity (severe). Co-administer with probenecid and IV saline to decrease toxicity.
- Coadminister cidofovir with probenecid
Anti-influenza Agents
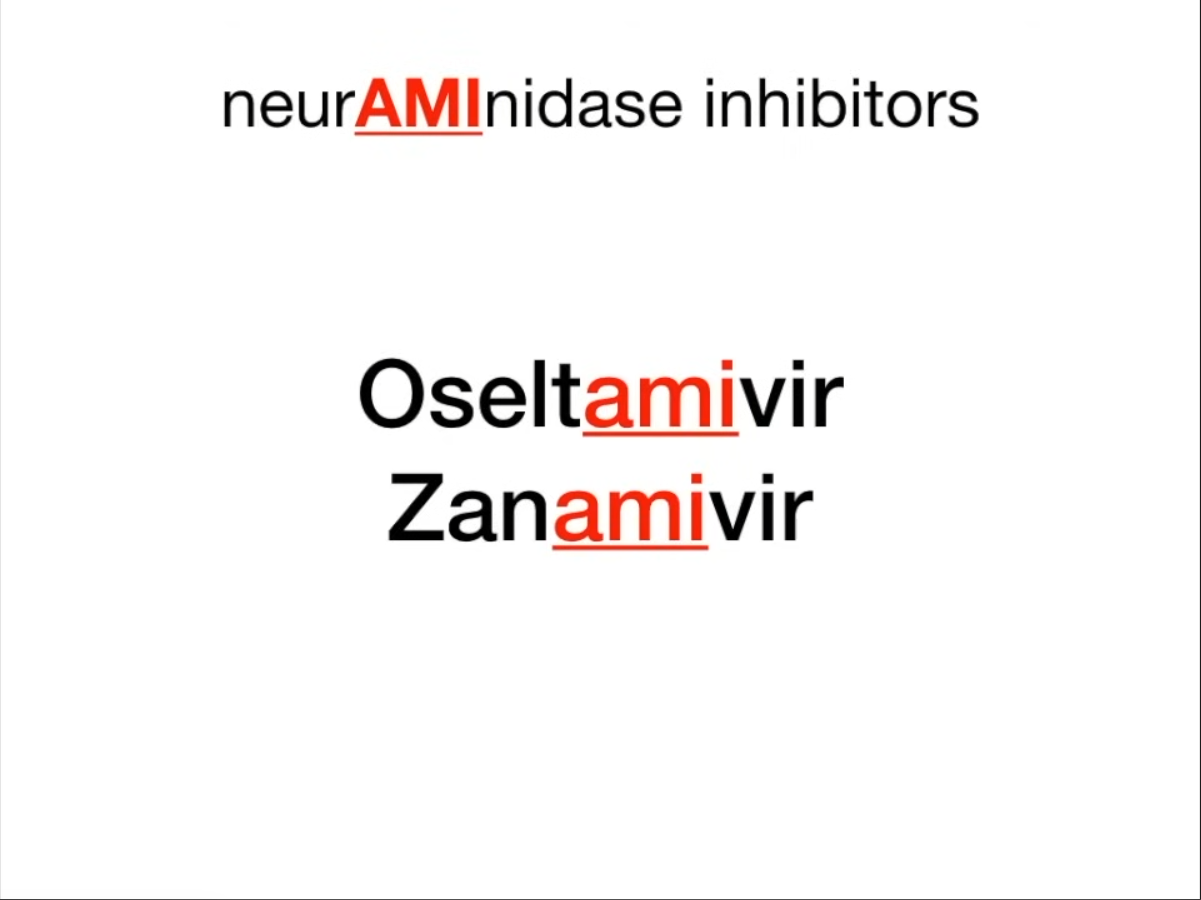
- Neuraminidase Inhibitors (Oseltamivir, Zanamivir)
- Mechanism: Inhibit influenza neuraminidase, preventing the release of progeny virions from infected cells. t
- Clinical Use: Treatment and prophylaxis of influenza. Must be given within 48 hours of symptom onset for maximal benefit.
- Adverse Effects: Oseltamivir: GI upset. Zanamivir: bronchospasm (avoid in asthma/COPD).
- Adamantanes (Amantadine, Rimantadine)
- Mechanism: Block the M2 proton channel, inhibiting viral uncoating.
- Clinical Use: Limited due to widespread resistance among influenza A strains. Not active against influenza B.
- Adverse Effects: CNS effects (ataxia, dizziness, slurred speech).
Anti-Hepatitis B & C Agents
- Hepatitis B (HBV) Tx
- Tenofovir, Entecavir, Lamivudine: Nucleos(t)ide reverse transcriptase inhibitors (NRTIs). Inhibit HBV DNA polymerase. Tenofovir and Entecavir are first-line due to low resistance rates.
- Interferon-alpha (IFN-α): Immunomodulatory effects. Used in younger patients with less advanced disease. Side effects include flu-like symptoms, depression, and autoimmune disorders.
- Hepatitis C (HCV) Tx - Direct-Acting Antivirals (DAAs)
- NS3/4A Protease Inhibitors (-previr; e.g., Glecaprevir): Inhibit the viral protease responsible for cleaving polyproteins.
- NS5A Inhibitors (-asvir; e.g., Ledipasvir, Velpatasvir): Inhibit NS5A, a phosphoprotein essential for viral replication and assembly.
- NS5B RNA Polymerase Inhibitors (-buvir; e.g., Sofosbuvir): Inhibit the viral RNA-dependent RNA polymerase.
- Management: Typically treated with a combination of 2-3 DAAs for >90% cure rate with minimal side effects.
- Ribavirin: Guanosine analog, inhibits viral RNA synthesis. Used in combination with other agents. Adverse effects: Hemolytic anemia, severe teratogen.