Two main categories: the very common adenocarcinoma and the less common but classic Pancreatic neuroendocrine tumors.
Epidemiology
- Age of onset: 60–80 years
Etiology
Exogenous risk factors
- Smoking (strongest risk factor)
- Considered to be one of the leading causes of pancreatic cancer and associated with an up to 6-fold increase in the risk of developing malignancy.
- Chronic pancreatitis (especially when present for more than 20 years)
- High alcohol consumption
- Type 2 diabetes mellitus
Endogenous risk factors
- Age > 50 years
- Inherited genetic syndromes (10% of pancreatic cancers)
- Familial atypical multiple mole melanoma (FAMMM) syndrome
- Hereditary breast and ovarian cancer syndrome (BRCA1 and BRCA2 mutations)
- HNPCC
- Von-Hippel-Lindau syndrome
- Neurofibromatosis type 1
- Multiple endocrine neoplasia type 1
- Familial pancreatic carcinoma
Clinical features
In most cases, there are no early symptoms suggestive of pancreatic cancer.
Gastrointestinal symptoms
- Belt-shaped epigastric pain which may radiate to the back
- Nausea
- Malabsorption, diarrhea (possibly steatorrhea secondary to exocrine pancreatic insufficiency)
- Jaundice caused by obstruction of extrahepatic bile ducts (especially in tumors of the pancreatic head)
- Courvoisier sign: enlarged, nontender gallbladder and painless jaundice
- Pale stools, dark urine, and pruritus
Hypercoagulability
- Trousseau syndrome: superficial thrombophlebitis (in 10% of cases) t
- Recurring thrombophlebitis in changing locations (migratory)
- Red, tender extremities
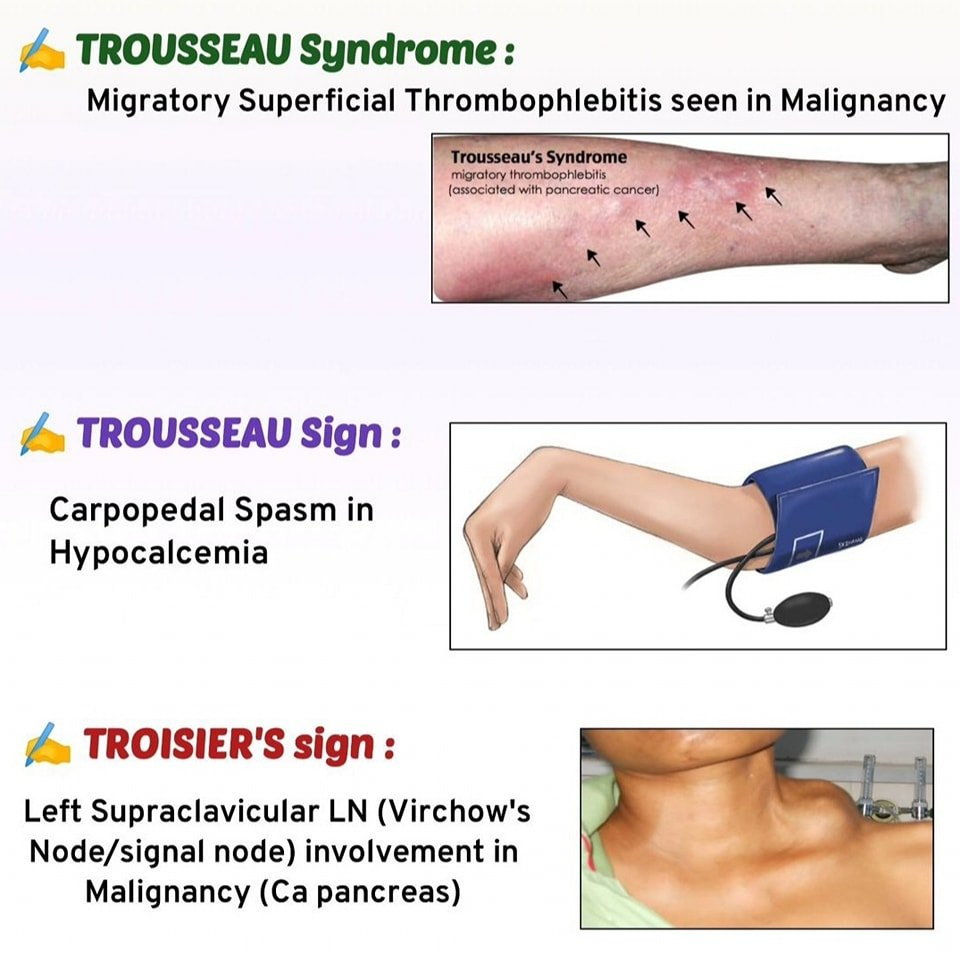
- Classically associated with pancreatic cancer
- Hypercoagulable state induced by tumor-secreted procoagulants
- Mucin-producing adenocarcinomas release tissue factor and mucin → activates coagulation cascade
- Results in recurrent, migratory venous thromboses
Tip
A thrombosis of unknown origin may be caused by an undiagnosed malignancy (especially pancreatic cancer, but also pulmonary, and prostatic carcinoma, the “3P’s”).
Warning
In the majority of instances, pancreatic cancer is diagnosed in symptomatic patients once it has already spread regionally or distally and is no longer resectable.
| Feature | Pancreatic Cancer | Cholangiocarcinoma |
|---|---|---|
| Key Hx | Smoking, chronic pancreatitis, new-onset DM | Primary Sclerosing Cholangitis (PSC), ulcerative colitis, pt from Asia |
| Exam Sign | Courvoisier sign (palpable, non-tender GB) | Gallbladder often not palpable (esp. with Klatskin tumor) |
| Systemic Sign | Trousseau syndrome (migratory thrombophlebitis) | Usually absent |
| Imaging | ”Double duct” sign (CBD + pancreatic duct dilation) | Isolated biliary duct dilation (normal pancreatic duct) |
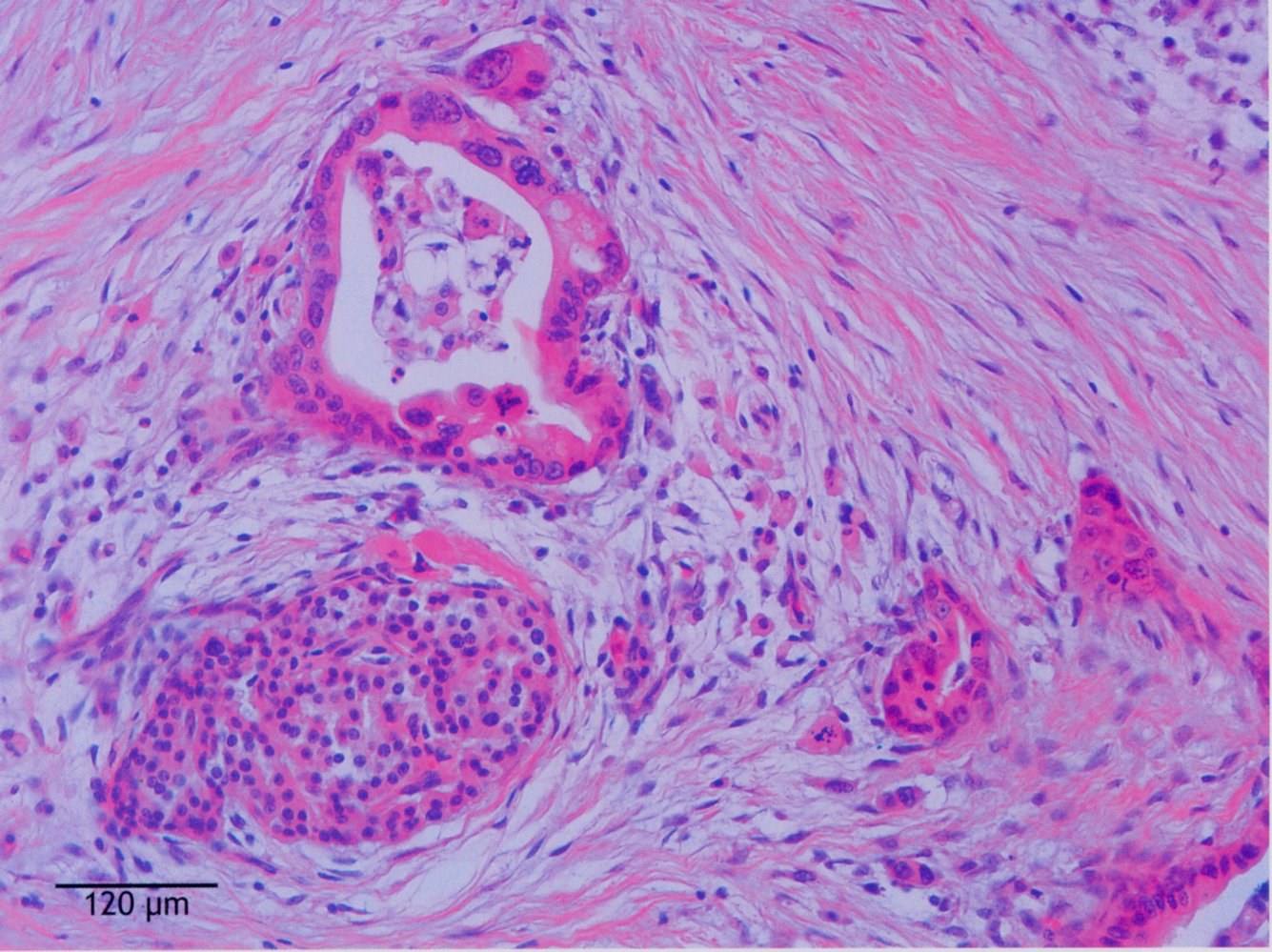
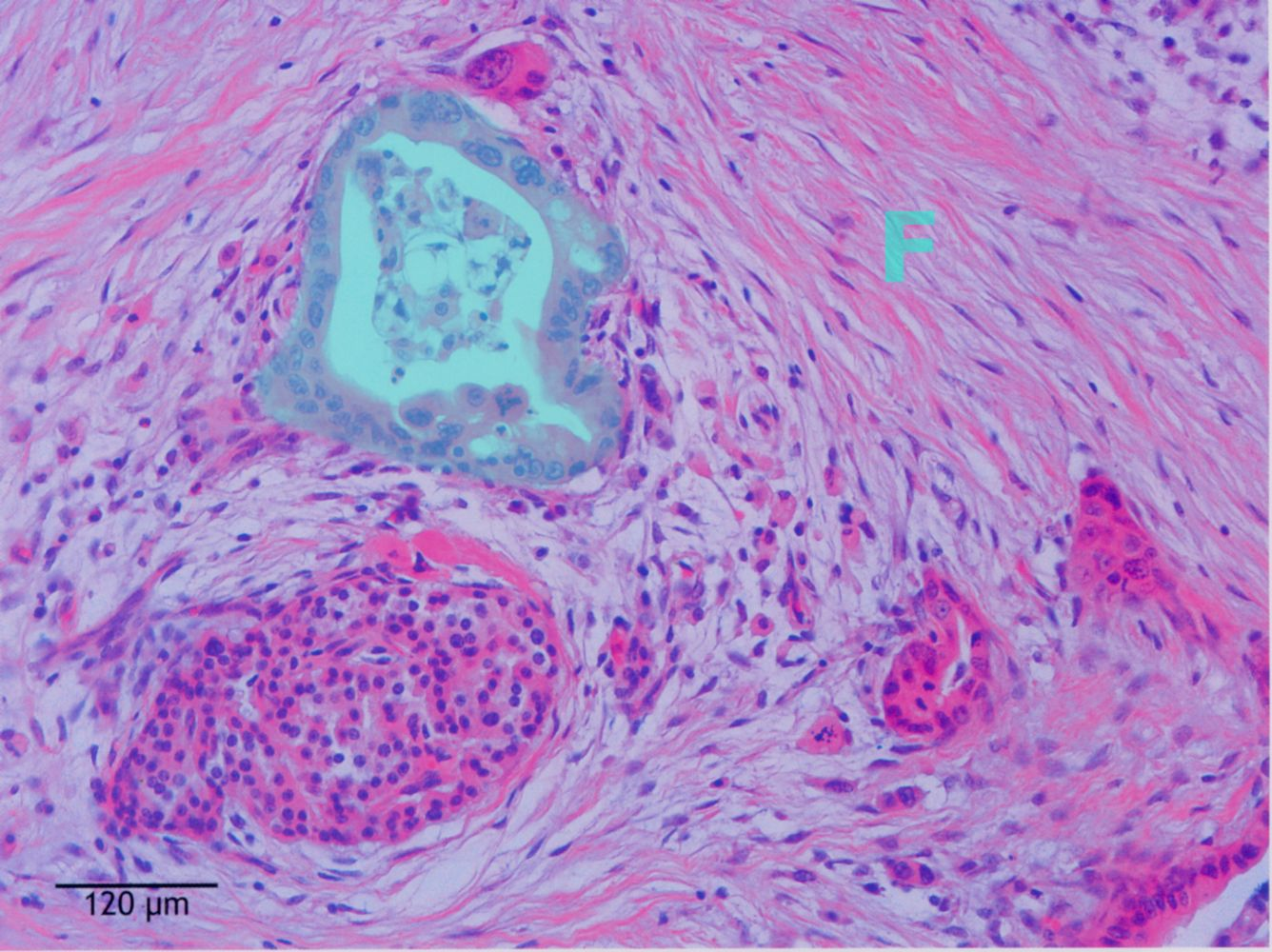
Pathology
- Histologic Type
- Invasive Ductal Adenocarcinoma (>90% of cases).
- Arises from pancreatic intraepithelial neoplasia (PanIN).
- Location
- Head of pancreas (60–70%): Compresses common bile duct → painless obstructive jaundice (Courvoisier sign).
- Body/Tail: often presents late (weight loss, pain) as they do not obstruct biliary tree early.
Cell origin
- Pancreatic exocrine tumors: originate from pancreatic acini and ducts
- Most common: ductal adenocarcinoma (95%)
- Altered ductal structures
- Cellular infiltration
- Adenocarcinoma of the pancreatic head is visible originating from the ductal cells, which have an atypical, uneven, multilayered epithelium (green overlay). F: fibrous septa
- Most common: ductal adenocarcinoma (95%)