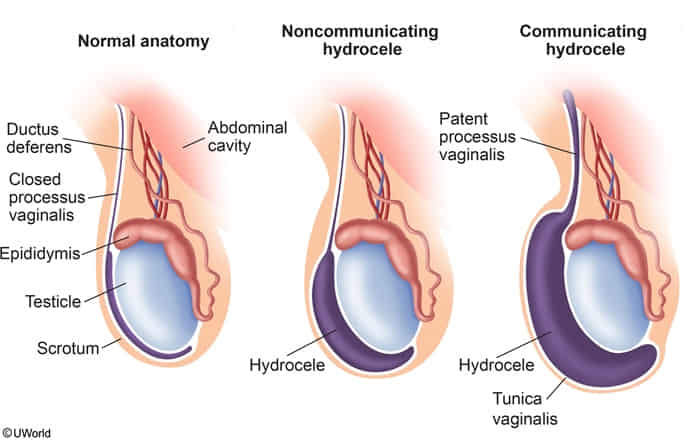
Hydrocele
- Patho/Etiology
- Collection of peritoneal fluid in the tunica vaginalis surrounding the testicle.
- Communicating: Caused by a patent processus vaginalis, allowing abdominal fluid to enter the scrotum. The size of the scrotal swelling may fluctuate.
- Non-communicating: Results from excess fluid production or impaired reabsorption within a closed tunica vaginalis, often due to inflammation or trauma.
- Very common in newborns and usually resolves spontaneously within the first year.
- Clinical Presentation
- Painless, cystic scrotal swelling that feels smooth and tense.
- May report a feeling of heaviness or discomfort if large.
- Diagnosis
- Transillumination: The mass will glow with a red hue when a light is shone through it, confirming its fluid-filled nature. This is a key diagnostic feature.
- Ultrasound: Used to confirm the diagnosis and rule out other pathology like testicular tumors or hernias, especially if the testis cannot be palpated.
- Management
- Infants: Observation. Most congenital hydroceles resolve spontaneously by age one.
- Adults/Persistent: Surgical correction (hydrocelectomy) is indicated if it is very large, symptomatic, or persists beyond 1-2 years of age in children.
Varicocele
- Patho/Etiology
- Dilation of the pampiniform plexus of spermatic veins, analogous to varicose veins in the leg.
- Caused by incompetent venous valves leading to retrograde blood flow and pooling.
- Overwhelmingly left-sided (~90%) because the left testicular vein drains into the left renal vein at a 90-degree angle, making it susceptible to compression (e.g., between the SMA and aorta—the “nutcracker effect”). The right testicular vein drains directly into the IVC. t
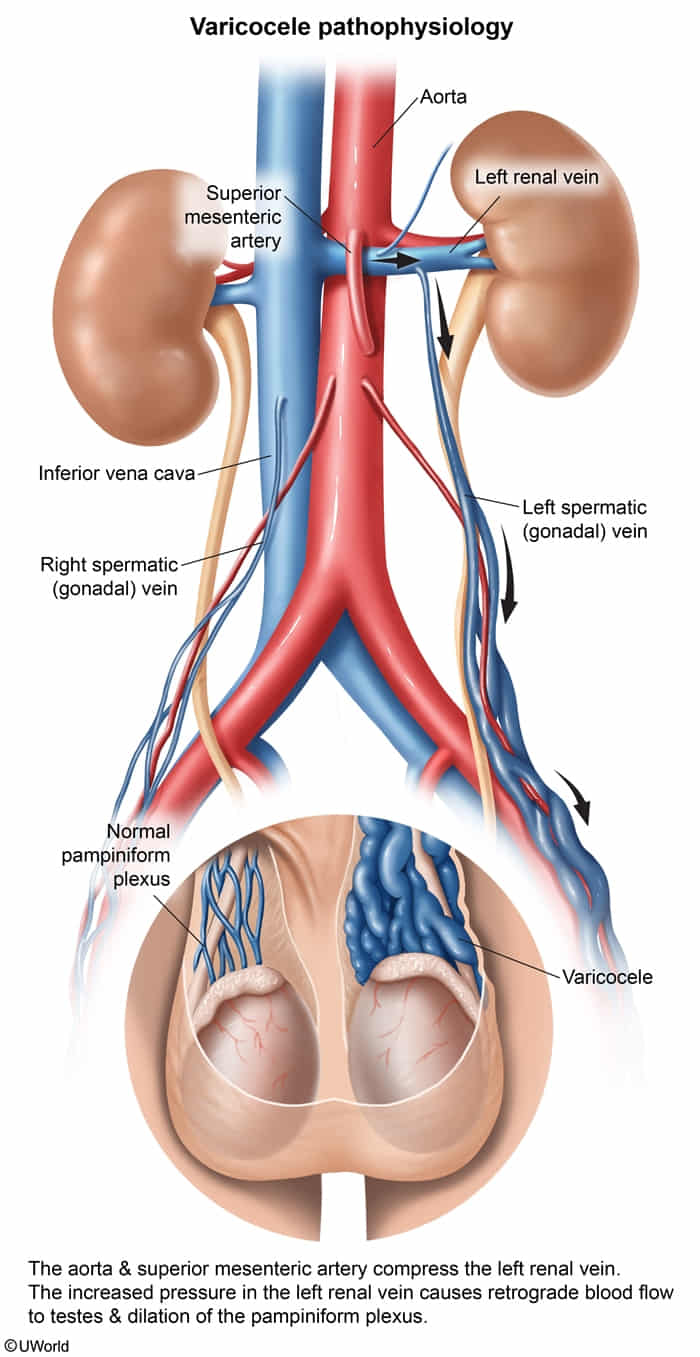
- A new-onset, right-sided varicocele is a red flag for retroperitoneal pathology (e.g., renal cell carcinoma with tumor thrombus) obstructing the IVC.
Tip
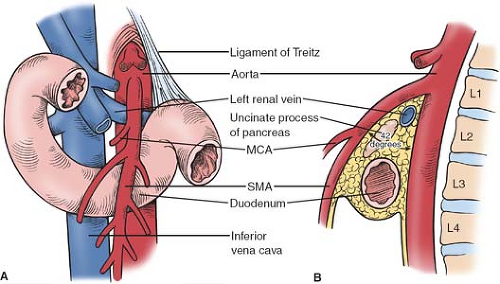
Superior mesenteric artery can compress both transverse duodenum (SMA Syndrome) and left renal vein (Nutcracker Syndrome)
- Clinical Presentation
- Often asymptomatic.
- Described as a scrotal mass that feels like a “bag of worms”.
- Dull, dragging, or aching scrotal pain, particularly worse with standing or at the end of the day, and relieved by lying down.
- Key association: Infertility. Increased temperature from pooled blood can impair spermatogenesis and cause testicular atrophy. t
- Diagnosis
- Physical Exam: Mass is palpable, especially with the Valsalva maneuver, which increases intra-abdominal pressure and venous distention.
- Does NOT transilluminate.
- You can shine a light through a sac of clear fluid (hydrocele), but you cannot shine a light through a bundle of veins filled with blood (varicocele). Blood is opaque. It is dense with red blood cells, proteins, and other components that block and absorb light.
- Ultrasound: Gold standard for diagnosis, showing dilated veins (>3 mm) and retrograde flow. Also used to assess testicular size.
- Management
- Asymptomatic varicoceles often require no treatment.
- Indications for Tx: Testicular atrophy, significant pain, or male infertility.
- Tx Options:
- Surgical varicocelectomy: Ligation of the spermatic veins.
- Percutaneous embolization: A less invasive radiologic procedure to block the vein.
Key Distinctions for USMLE
| Feature | Hydrocele | Varicocele |
|---|---|---|
| Pathology | Peritoneal fluid in tunica vaginalis | Dilated pampiniform venous plexus |
| Palpation | Smooth, cystic, tense | ”Bag of worms” |
| Transillumination | Positive (glows) | Negative (opaque) |
| Effect of Valsalva | Communicating can increase in size; non-com doesn’t | Increases in size |
| Effect of Position | Size is stable (non-communicating) or may decrease with lying down (communicating) | Decreases/disappears when lying down |
| Key Association | Patent processus vaginalis | Infertility, left-sided predominance |