Epidemiology
Etiology
- Central DI (CDI): Decreased or absent ADH production/secretion from the posterior pituitary.
- Causes: Most commonly idiopathic, but can result from head trauma, pituitary surgery, tumors (e.g., craniopharyngioma), or infiltrative diseases like sarcoidosis.
- High-Yield Note: Damage to the posterior pituitary usually causes transient DI; permanent DI requires damage to the hypothalamic nuclei (supraoptic/paraventricular). t
- Nephrogenic DI (NDI): Renal insensitivity to ADH. The kidneys do not respond appropriately to normal ADH levels.
- Causes: Most commonly caused by medications, especially Lithium. Other causes include genetic mutations in the V2 receptor or aquaporin-2 channels, hypercalcemia, and hypokalemia.
Pathophysiology
Tip
Note that in central DI, ADH levels are decreased, while in nephrogenic DI, they are normal or increased to compensate for the high urine output.
Clinical features
- Polyuria with dilute urine
- Nocturia → restless sleep, daytime sleepiness
- Polydipsia (excessive thirst)
- In cases of low water intake → severe dehydration (altered mental status, lethargy, seizures, coma) and hypotension
- Symptoms may worsen during pregnancy.
Tip
In the absence of nocturia, diabetes insipidus is very unlikely.
Diagnostics
- Initial Labs: High serum osmolality (>295 mOsm/kg), low urine osmolality (<300 mOsm/kg), and hypernatremia (Na+ >145 mEq/L) despite polyuria.
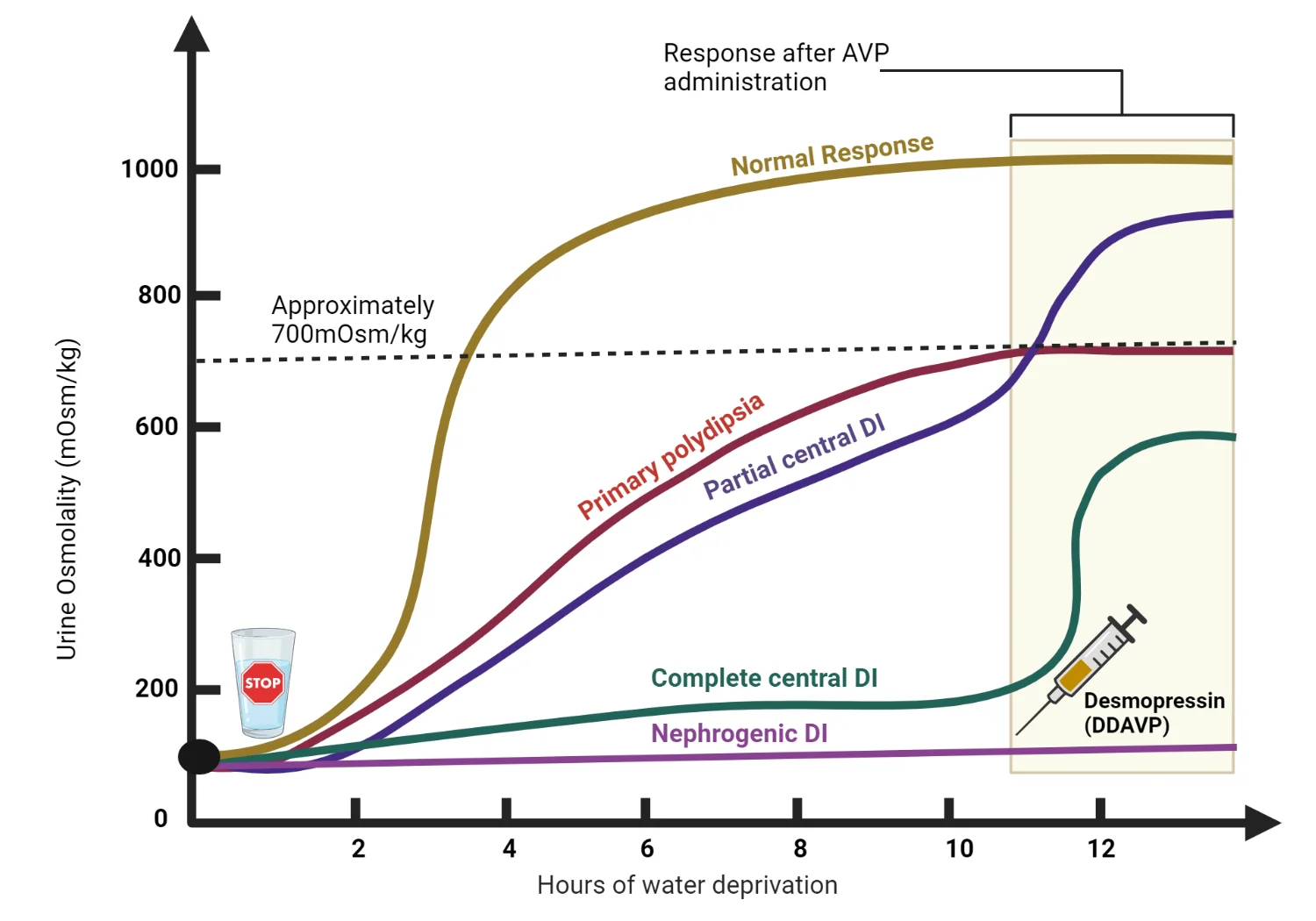
- Water Deprivation Test: The key diagnostic test to differentiate DI from primary polydipsia. The patient is deprived of fluids, and urine osmolality is measured.
- Desmopressin (ADH analog) Stimulation Test: This follows the water deprivation test to distinguish between CDI and NDI.
- Central DI: Urine osmolality remains low during water deprivation but significantly increases (>50% increase) after desmopressin administration.
- Nephrogenic DI: Urine osmolality stays low after both water deprivation and desmopressin administration.
- Primary Polydipsia: Urine osmolality increases appropriately with water deprivation alone, as the ADH system is intact.
Serum sodium and plasma osmolality
- ↓ Na+ and/or ↓ plasma osmolality: primary polydipsia likely
- Normal values: diagnosis unclear; obtain subsequent studies to differentiate between polyuria-polydipsia syndromes.
- ↑ Na+ and/ or ↑ plasma osmolality: Diabetes insipidus likely; obtain subsequent studies to differentiate between CDI and NDI.
Differential diagnostics
Primary polydipsia (psychogenic polydipsia)
- Mechanism
- Compulsive water intake
- Etiology
- Psychiatric diseases (e.g., schizophrenia, obsessive-compulsive disorder)
- Lesions in the hypothalamic thirst center
- Features
- Hyponatremia
- Low plasma osmolarity, very low urine osmolarity
- Water deprivation: plasma and urine osmolarity increase to normal level
Treatment
- Central DI:
- Desmopressin (DDAVP): A synthetic ADH analog is the first-line treatment. It can be administered intranasally, orally, or parenterally.
- Nephrogenic DI:
- Address underlying cause: Discontinue offending drugs like lithium.
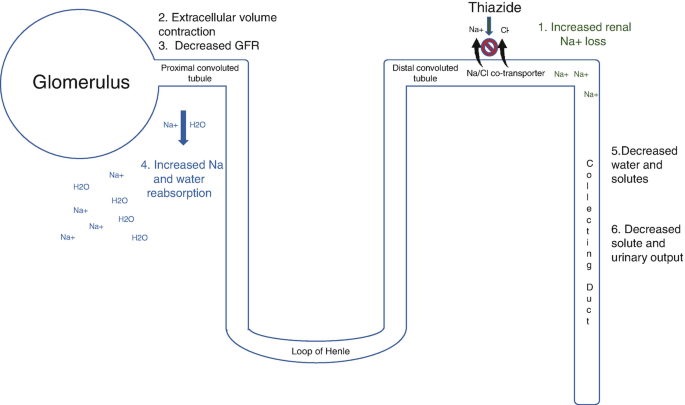
- Thiazide Diuretics (e.g., HCTZ): Paradoxically reduce urine output by promoting water reabsorption in the proximal tubules. t
- Low-sodium diet: Reduces the osmotic load on the kidneys.
- Amiloride: Useful for lithium-induced NDI as it can block lithium entry into renal collecting duct cells.