Sleep physiology
Mnemonic
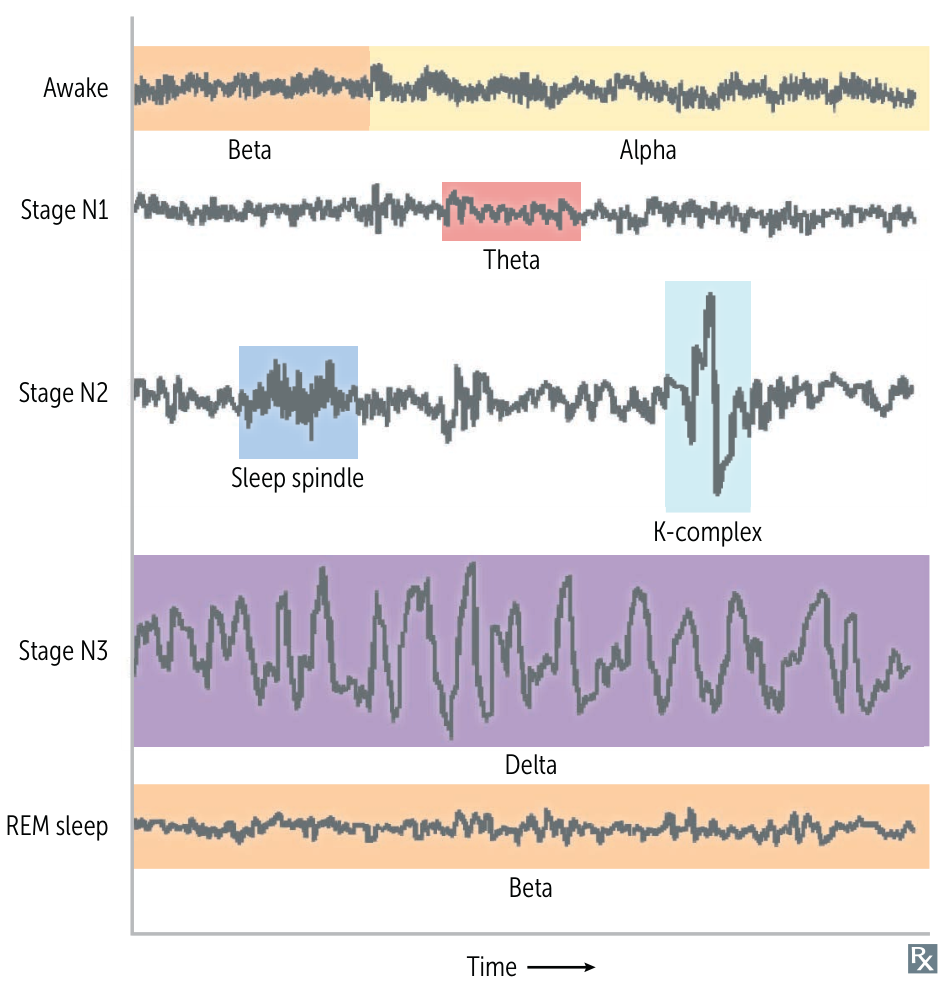
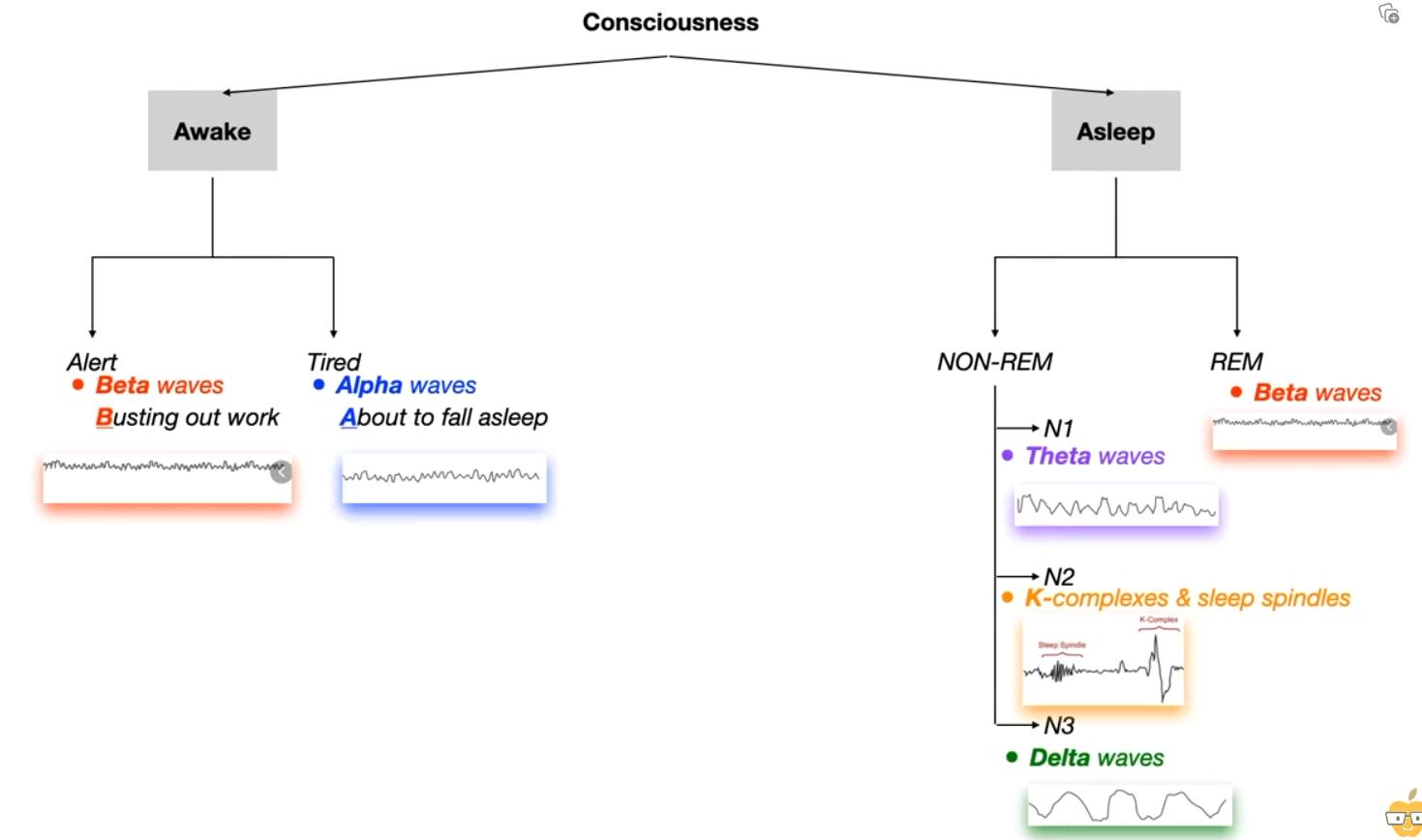
EEG waveforms: Beta, Alpha, Theta, Sleep spindle, Delta, Beta. At night, BATS Drink Blood.
Tip
Alert and REM are both Beta waves.
Non-REM (NREM) Sleep
-
N1 (Light Sleep)
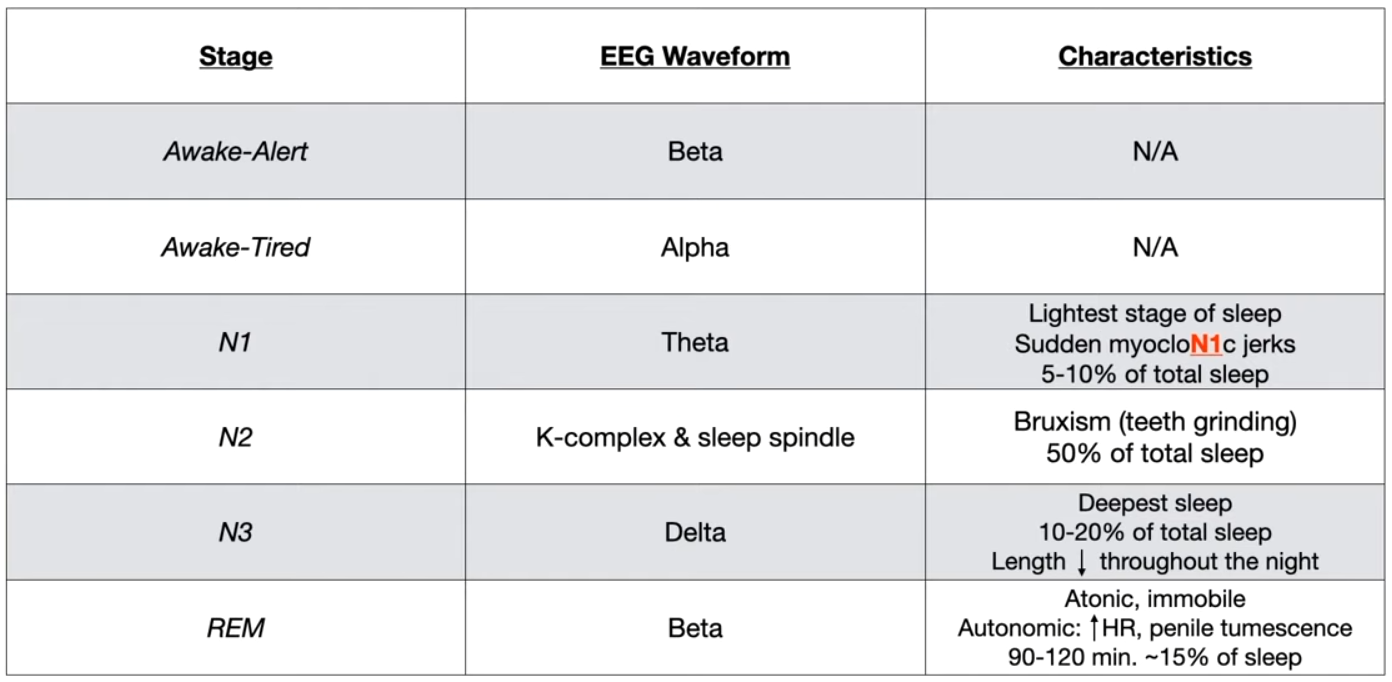
- EEG: Theta waves.
- Description: Transition from wakefulness to sleep (5% of total sleep). Very light sleep from which one is easily awakened.
- Physiology: Slow, rolling eye movements.
-
N2 (Intermediate Sleep)
- EEG: Sleep spindles and K-complexes on a background of theta waves.
- Description: Largest percentage of total sleep time (~45-55%). Deeper sleep than N1.
- Key Associations: Bruxism (teeth grinding) often occurs during this stage.
-
N3 (Deep Sleep / Slow-Wave Sleep)
- EEG: Delta waves (low frequency, high amplitude).
- Description: Deepest stage of sleep (~10-20% of total sleep), most difficult to awaken from. Most prominent in the first half of the night.
- The brain is “asleep” (high arousal threshold), but the motor system is not paralyzed, allowing for complex movements. This is why parasomnias like sleepwalking (somnambulism) and night terrors occur during N3.
- N3 sleep is considered the most physically restorative stage. During this time, the body focuses on repair and growth, such as tissue repair, bone and muscle building, and strengthening the immune system.
- Key Associations: Parasomnias such as somnambulism (sleepwalking), night terrors, and bedwetting (enuresis) occur here.
REM (Rapid Eye Movement) Sleep
- EEG: Beta waves (high frequency, low amplitude), similar to the awake state; “sawtooth waves” are also characteristic.
- Description: “Paradoxical sleep” as the brain is highly active while the body is immobile (~20-25% of total sleep). Duration of REM periods increases with each cycle throughout the night.
- Not the “Deepest”: Although you are paralyzed, your arousal threshold during REM sleep is actually lower than in N3 sleep. It is generally easier to wake someone from REM sleep. When awakened from REM, people often feel alert and can vividly recall their dreams, unlike the grogginess (“sleep inertia”) experienced when woken from N3.
- Physiology:
- Rapid eye movements.
- Atonia: Generalized muscle paralysis (except for extraocular muscles and diaphragm). This is protective, preventing one from acting out dreams.
- Vivid dreaming and nightmares occur.
- Variable heart rate and blood pressure, penile/clitoral tumescence.
- Key Associations:
- Important for memory consolidation.
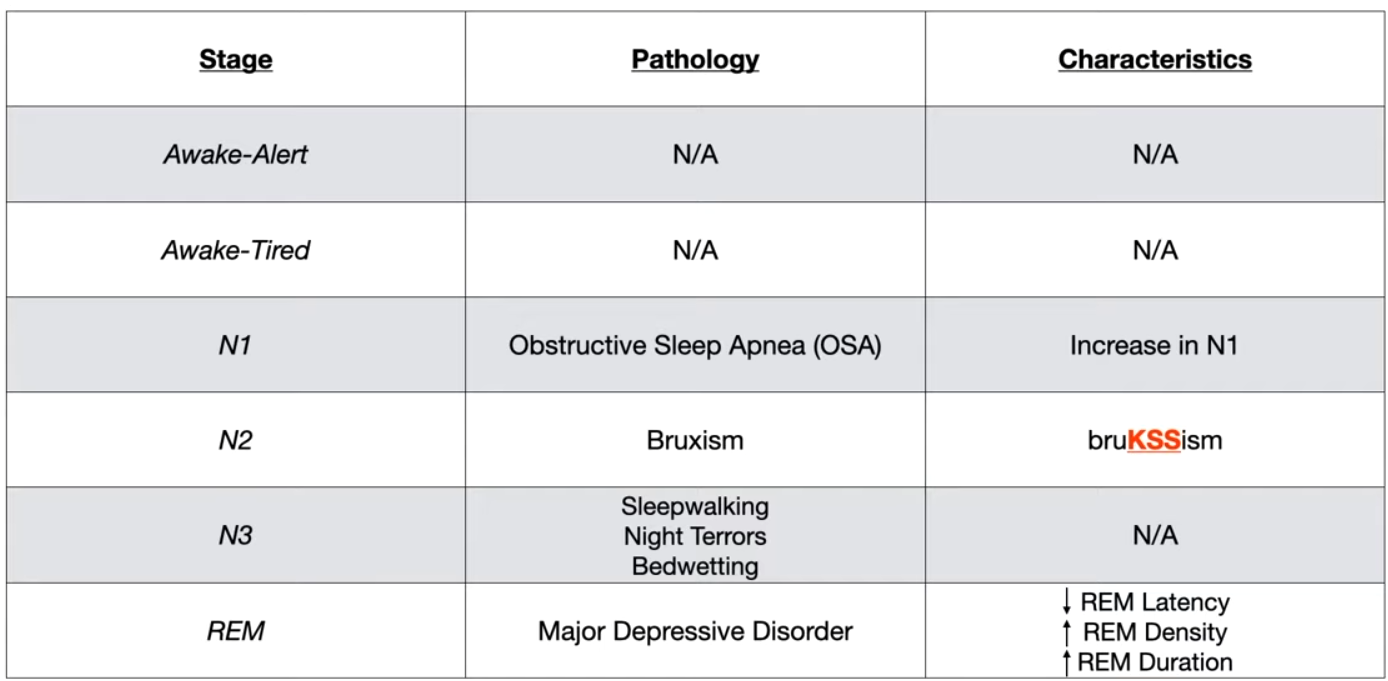
- Depression is associated with increased total REM sleep and decreased REM latency (earlier onset of REM).
- REM sleep behavior disorder: Loss of atonia leads to dream enactment (e.g., punching, kicking).
Mnemonic
- In REM stage, B for Beta and Boner.
- REMember your dream
- REMain still (so you won’t act like in dreams)
- To remember K complex and Sleep Spindle is N2
- It takes ‘2’ to “KiSS” (also note that kissing involves mouth and hence teeth=Teeth grinding)
- Delta for Deepest sleep
Mnemonic
- N1: Obstructive Sleep ApN1a
- N3: wee and flee in N3
- REM: In MDD you have less fine, deep sleep (N3), more REM.
Tip
- Obstructive sleep apnea
- Leads to an increased percentage of N1 sleep
- Because the frequent arousals prevent the individual from consolidating deeper stages of sleep (N2, N3/slow-wave sleep, and REM sleep).
- The most severe individual apnea/hypopnea events (longest duration, greatest oxygen desaturation) are most likely to occur during REM sleep
- Because of loss of muscle tone (atonia) in REM
Sleep disorders
Dyssomnias (Disorders of Sleep Amount/Timing)
Obstructive Sleep Apnea (OSA)
- Patho: Upper airway collapse → apnea/hypopnea → hypoxia.
- Presentation: Obese patient (BMI > 30), excessive daytime sleepiness, loud snoring, morning headaches.
- Dx: Polysomnography.
- Tx: CPAP is first-line; weight loss.
- Complications: Systemic HTN, pulmonary HTN, arrhythmias.
Narcolepsy
- Patho: ↓ Orexin (hypocretin) from lateral hypothalamus.
- Presentation: Excessive daytime sleepiness, cataplexy (sudden muscle tone loss with strong emotion), hypnagogic/hypnopompic hallucinations, sleep paralysis.
- Dx: Multiple Sleep Latency Test (MSLT) shows ↓ sleep latency and sleep-onset REM.
- Tx: Modafinil for sleepiness; SSRIs/SNRIs for cataplexy.
Restless Legs Syndrome (RLS)
- Patho: Associated with iron deficiency and CNS dopamine dysfunction.
- Presentation: Overwhelming urge to move legs, worse at night/rest, relieved by movement.
- Dx: Clinical; check ferritin.
- Tx: Treat iron deficiency. First-line drugs are alpha-2-delta ligands (e.g., Gabapentin) or dopamine agonists (e.g., Pramipexole).
Circadian rhythm sleep-wake disorders
- Etiology/Pathophysiology
- Misalignment between the endogenous circadian clock and the external 24-hour light-dark cycle.
- The master clock is the suprachiasmatic nucleus (SCN) in the hypothalamus, which regulates the sleep-wake cycle.
- The SCN is primarily entrained by light cues from the retina. Other cues (zeitgebers) include meals and exercise.
- The SCN controls the pineal gland’s release of melatonin, which signals darkness and promotes sleep. Melatonin is synthesized from serotonin, which comes from tryptophan.
- Can be intrinsic (alteration of the clock itself) or extrinsic (misalignment with social/work schedules).
- Types of Circadian Rhythm Sleep-Wake Disorders (CRSWD)
- Delayed Sleep-Wake Phase Disorder (DSWPD)
- Presentation: “Night owls.” Inability to fall asleep at a desired conventional time, leading to difficulty waking in the morning. Sleep is normal if allowed to follow their own schedule (e.g., sleeping 2 AM to 10 AM).
- Epidemiology: Common in adolescents and young adults.
- Treatment: Morning bright light therapy to advance the sleep phase (shift it earlier). Evening administration of melatonin.
- Advanced Sleep-Wake Phase Disorder (ASWPD)
- Presentation: “Early birds.” Sleepiness and sleep onset are several hours earlier than desired, leading to early morning awakenings.
- Epidemiology: More common in older adults.
- Treatment: Evening bright light therapy to delay the sleep phase (shift it later). Morning administration of melatonin can also delay the phase.
- Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD)
- Presentation: A free-running rhythm where the sleep-wake cycle is not entrained to 24 hours, typically shifting later each day. Pts experience periods of insomnia and sleepiness that cyclically align and misalign with the day-night cycle.
- Epidemiology: Most common in individuals who are totally blind due to the lack of light input to the SCN.
- Treatment: Melatonin to help entrain the rhythm. Melatonin receptor agonists (e.g., tasimelteon) are FDA-approved.
- Irregular Sleep-Wake Rhythm Disorder (ISWRD)
- Presentation: Lack of a discernible circadian rhythm. Sleep is fragmented into multiple naps throughout a 24-hour period. Pts complain of both insomnia and excessive sleepiness.
- Epidemiology: Often associated with neurodegenerative diseases (e.g., Alzheimer’s dementia) or brain injury affecting the SCN.
- Treatment: Focuses on structured daily routines, consolidating sleep, and timed light exposure and melatonin.
- Shift Work Disorder
- Presentation: Insomnia and excessive sleepiness due to a work schedule (e.g., night shifts) that conflicts with the endogenous circadian rhythm.
- Epidemiology: Affects up to a third of shift workers.
- Treatment: Improving sleep hygiene, planned naps before shifts, and sometimes wakefulness-promoting agents (e.g., modafinil).
- Jet Lag Disorder
- Presentation: Transient misalignment of the internal clock with the new time zone after rapid travel across at least two time zones.
- Symptoms: Insomnia, daytime sleepiness, and somatic complaints like GI upset.
- Details: Eastward travel (advancing one’s clock) is generally more difficult to adjust to than westward travel.
- Treatment: Short-acting hypnotics or low-dose melatonin can be used. Timed light exposure is key to adapting to the new time zone.
- Delayed Sleep-Wake Phase Disorder (DSWPD)
- Diagnostics
- Clinical History: The cornerstone of diagnosis, focusing on sleep schedules, work/social obligations, and symptoms. Symptoms should typically be present for at least 3 months.
- Sleep Diary/Log: A detailed record of sleep and wake times over 1-2 weeks is crucial to identify patterns.
- Actigraphy: A wrist-worn device that measures activity and rest over several days to objectively estimate sleep-wake patterns.
- Dim Light Melatonin Onset (DLMO): Salivary or plasma measurements can identify the timing of the endogenous circadian rhythm, but this is primarily a research tool.
- General Treatment Principles
- Sleep Hygiene: Maintaining a regular sleep-wake schedule (even on weekends), creating a dark and quiet sleep environment, and avoiding caffeine/alcohol before bed.
- Light Therapy (Phototherapy): The most potent stimulus for entraining the circadian clock.
- Morning light causes a phase-advance (shifts clock earlier).
- Evening light causes a phase-delay (shifts clock later).
- Melatonin: Exogenous melatonin can shift the circadian phase.
- Evening administration (several hours before desired bedtime) causes a phase-advance.
- Morning administration causes a phase-delay.
Parasomnias (Abnormal Events During Sleep)
NREM Parasomnias
- Occur during N3 (deep) sleep; person is difficult to arouse and has no memory of event. More common in children.
- Sleep Terrors: Abrupt screaming/fear, inconsolable.
- Sleepwalking (Somnambulism): Motor activity during sleep.
REM Parasomnias
- Occur during REM sleep; person can be aroused and often recalls the event.
- Nightmare Disorder: Frightening dreams followed by full alertness upon waking.
- REM Sleep Behavior Disorder (RBD): Dream-enactment behavior due to lack of muscle atonia. Strong predictor for future α-synucleinopathies (e.g., Parkinson disease).
Parasomnias
Sleep terror disorder
- Definition: a non-REM-related parasomnia that occurs during the N3 sleep stage (slow-wave sleep), characterized by episodes of sleep terror
- Epidemiology: Discrete episodes of sleep terrors are relatively common in children (∼ 20% of children and ∼ 2% of adults), but the disorder is rare.
- Risk factors
- Stress or fatigue
- Fever
- Sleep deprivation
- Clinical features
- Screaming or crying suddenly upon awakening, usually in the first part of the night (rarely during daytime naps)
- Intense fear and agitation
- Tachypnea, diaphoresis, tachycardia during episodes
- Difficulty arousing patients during episodes
- Patients usually return to sleep after the episode.
- Typically no recollection of the arousal episode (unlike with nightmare disorder)
- Nightmare disorder
- a REM-related parasomnia characterized by recurrent nightmares
- Patient remembers the dream after awakening (REMember)
- Nightmare disorder
REM sleep behavior disorder
- Definition: a REM-related parasomnia characterized by dream enactment due to loss of REM sleep atonia
- Epidemiology
- Sex: ♂ > ♀
- Usually in older patients (> 50 years)
- Risk factors
- Narcolepsy
- Psychiatric medications (e.g., antidepressants)
- Neurodegenerative disorders (e.g., Parkinson disease, Lewy body dementia)
- Clinical features
- Physically acting out dreams during sleep (e.g., yelling, moving limbs, walking, punching), sometimes leading to injury to self or others
- Patient is alert and orientated after awakening, and remembers the dream.
- Prognosis: Most patients with idiopathic RBD eventually develop a disorder of α-synuclein neurodegeneration, most commonly Parkinson disease.