1. Opioid Intoxication (Overdose)
- Opioid overdose is the most common cause of drug overdose death.
- Pathophysiology
- Agonism of mu () receptors in CNS modulation of synaptic transmission (closing voltage-gated Ca channels presynaptically, opening K channels postsynaptically).
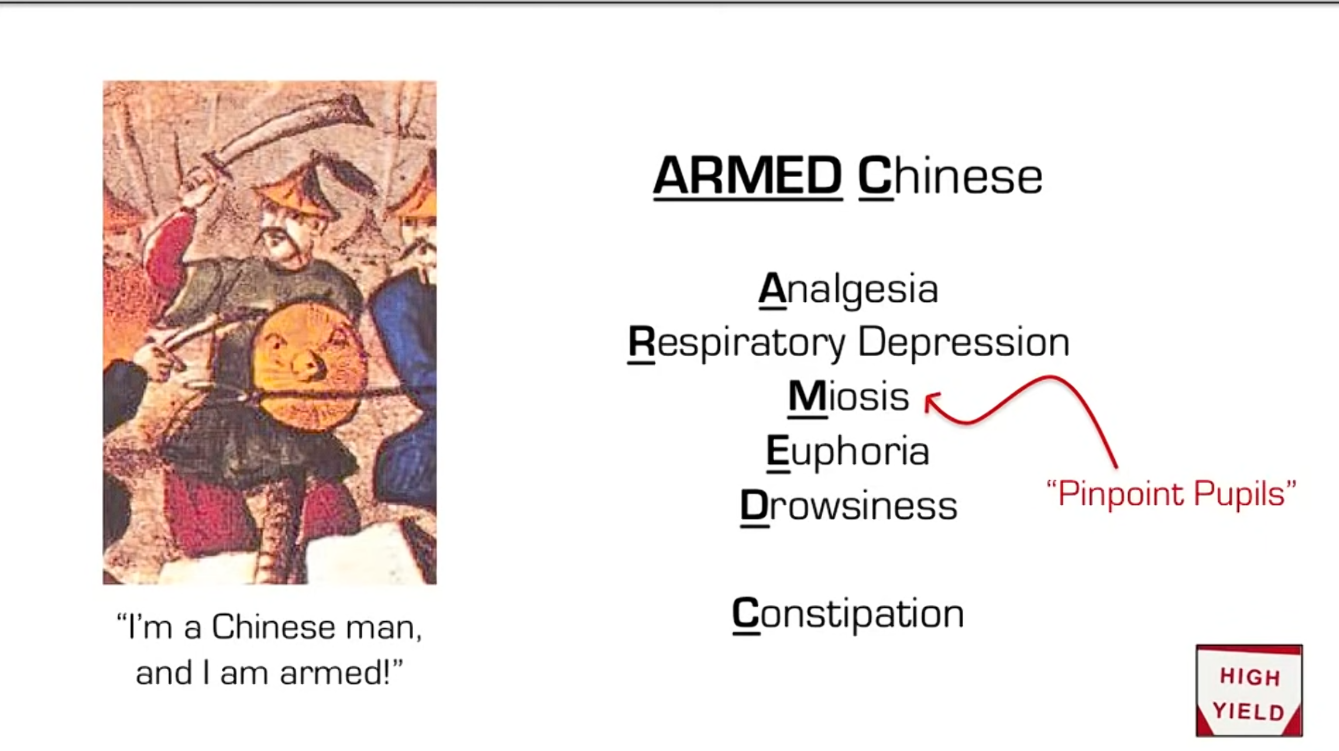
- Clinical Features
- Classic Triad:
- Respiratory Depression (RR < 12/min is the best predictor of toxicity).
- CNS Depression (lethargy, coma).
- Miosis (Pinpoint pupils).
- Other findings: bowel sounds, hypotension, bradycardia, hypothermia, hyporeflexia.
- Key Exception: Meperidine causes mydriasis (dilated pupils) due to anticholinergic effects and carries a risk of Serotonin Syndrome + Seizures.
- Classic Triad:
Warning
The absence of miosis does not rule out opioid overdose as hypoxia, co-ingested drugs (e.g., cocaine, amphetamines), and/or medications (e.g., atropine) may cause mydriasis, thereby counteracting the miotic effect of opioids.
- Treatment
- Airway protection (ABCs) is priority #1.
- Naloxone (Opioid antagonist): IV, IM, or Intranasal.
- Short half-life; may require redosing to prevent re-sedation.
- Short half-life; may require redosing to prevent re-sedation.
2. Opioid Withdrawal
- Pathophysiology
- Cessation of mu-agonism Noradrenergic hyperactivity (Locus ceruleus).
- Clinical Features
- Timeline: Starts 6–12 hrs after last dose (short-acting) or 24–48 hrs (long-acting).
- GI: Diarrhea, nausea, vomiting, abdominal cramping.
- Autonomic/CNS: Dilated pupils (mydriasis), piloerection (“cold turkey”), diaphoresis, tachycardia, hypertension.
- Specific Signs: Yawning, lacrimation, rhinorrhea.
- Note: Withdrawal is not life-threatening in adults (unlike alcohol/benzo withdrawal), but is extremely uncomfortable.
Mnemonic
Opioid yawning
- Neonatal Abstinence Syndrome (NAS)
- Neonate born to opioid-dependent mother.
- Sx: High-pitched cry, tremors, seizures, sneezing, poor feeding, diarrhea.
- Tx: Swaddling/calm environment; if severe, Morphine or Methadone.
- Management
- Symptomatic: Clonidine/Lofexidine (-agonists to blunt sympathetic surge), Loperamide (diarrhea), NSAIDs.
- Substitution: Buprenorphine or Methadone taper.
Mnemonic
- Methadone? The recovering heroin addict I met had one .
- Buprenorphine boops the morphine
Warning
Naloxone is for opioids overdose. Giving naloxone for acute opioid withdrawal or neonatal abstinence syndrome will result in more severe withdrawal symptoms and is contraindicated.
3. Opioid Use Disorder (OUD) Management
Long-term Pharmacotherapy (Medication-Assisted Treatment) is standard of care to reduce cravings and relapse risk.
- Methadone
- Mechanism: Long-acting full mu-agonist.
- Pros: Good for patients with high tolerance; suppresses cravings well.
- Cons: Very long half-life (risk of accumulation/OD); QT prolongation; requires daily visits to a registered clinic (stigma/inconvenience).
- Buprenorphine
- Mechanism: Partial mu-agonist.
- Pros: Ceiling effect (lower risk of respiratory depression); can be prescribed in office setting.
- Cons: Can precipitate withdrawal if given too soon (must wait for mild withdrawal symptoms before induction).
- Note: Often combined with Naloxone (Suboxone) to prevent IV abuse (Naloxone is not active orally/sublingually, but blocks effect if crushed and injected).
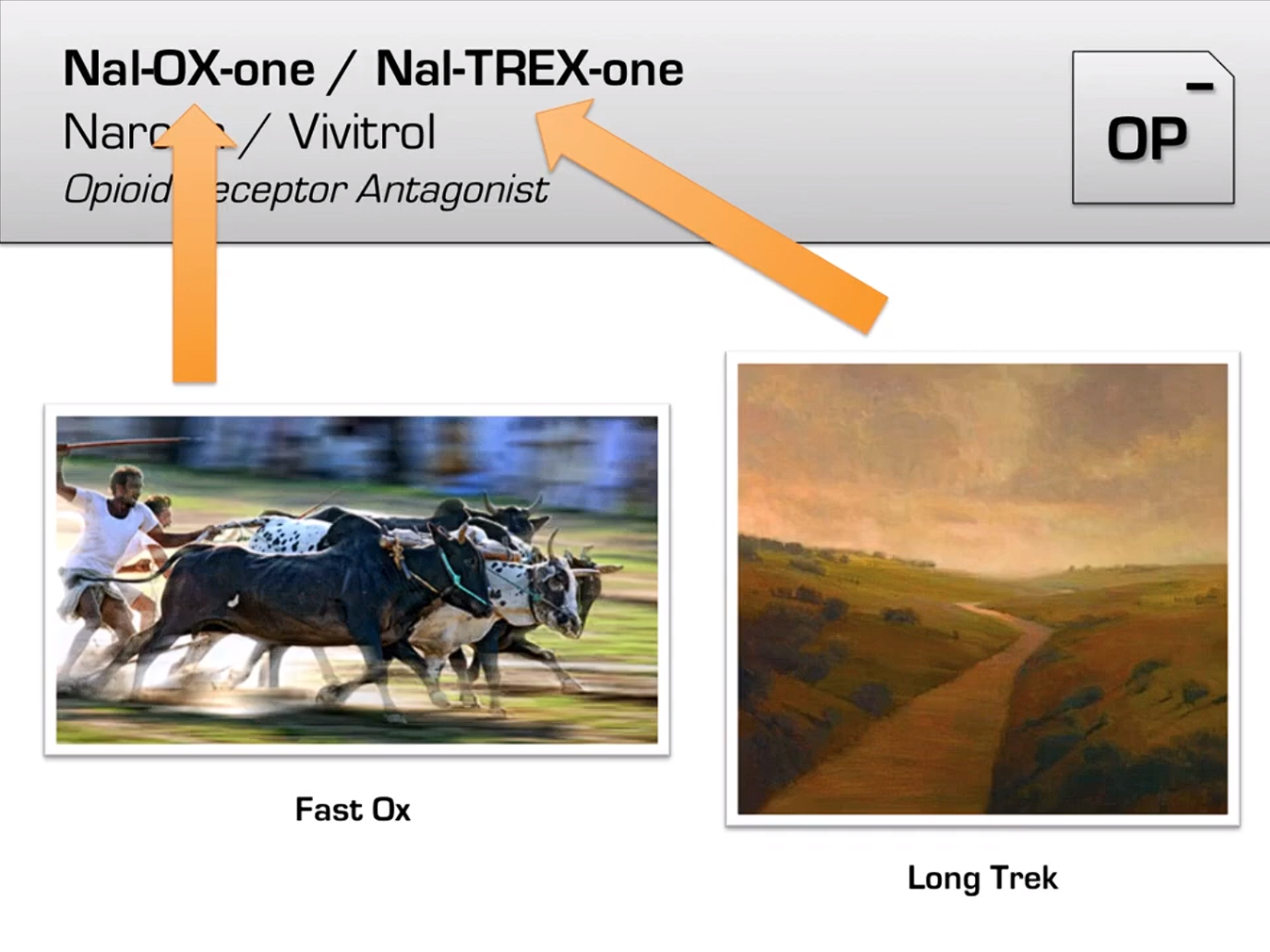
- Naltrexone
- Mechanism: Long-acting opioid antagonist (IM injection Vivitrol).
- Pros: Blocks euphoric effects if patient relapses; no physical dependence.
- Cons: Patient must be fully detoxified (7–10 days opioid-free) before starting, or it will cause severe precipitated withdrawal.
High-Yield Pharmacology Buzzwords
- Loperamide: Antidiarrheal; mu-agonist that does not cross the Blood-Brain Barrier (low abuse potential).
- Dextromethorphan: Antitussive; NMDA antagonist at high doses (abuse potential). can cause Serotonin Syndrome.
- Tramadol: Weak mu-agonist + inhibits 5-HT/NE reuptake. Risk of Seizures and Serotonin Syndrome.
- Codeine: Prodrug metabolized to morphine by CYP2D6. Ultra-rapid metabolizers (genetics) risk toxicity.