Combination usage
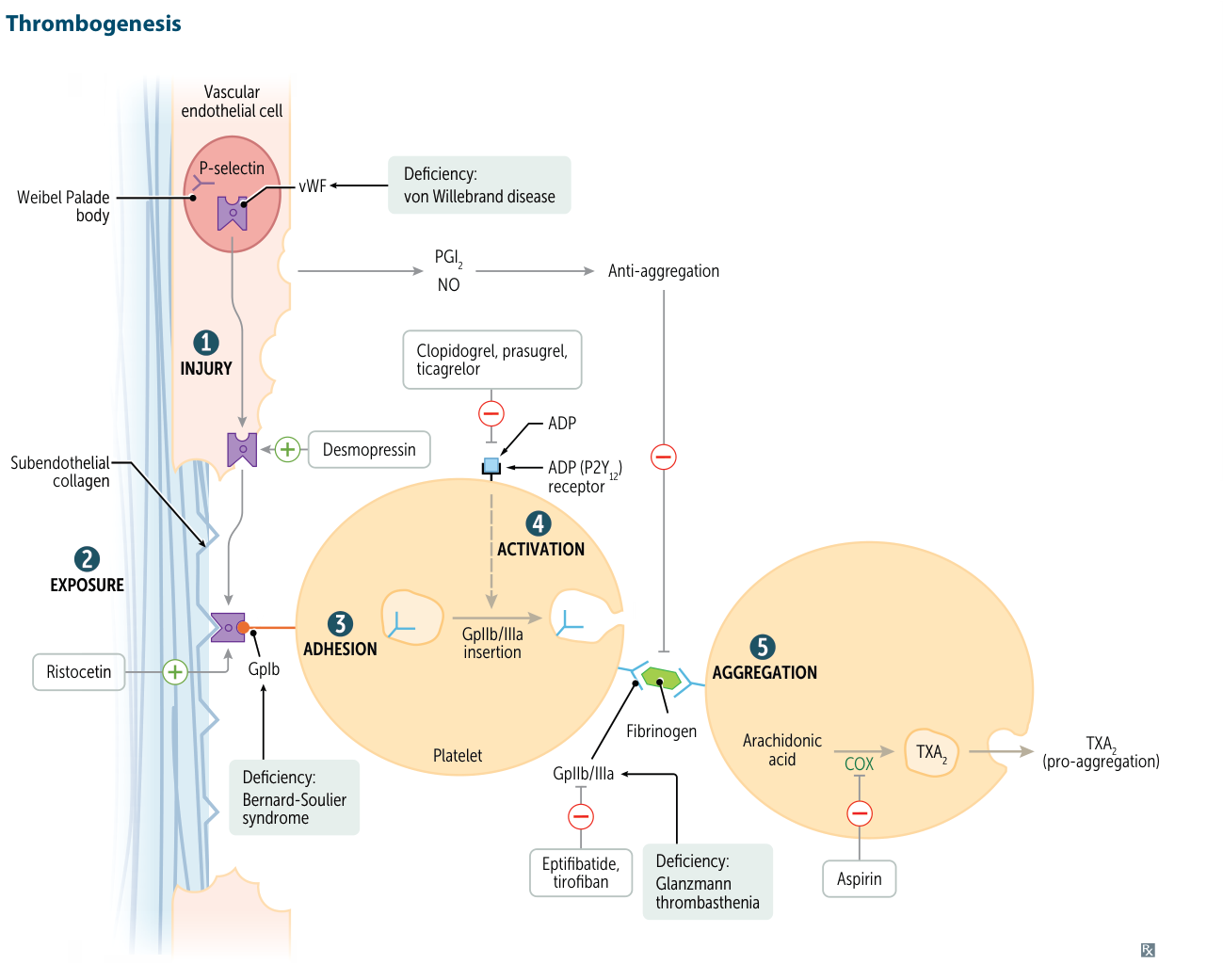
- The most common and important combination is DAPT (Aspirin + P2Y12 inhibitor) for ACS and coronary stents.
- Adding an anticoagulant creates “Triple Therapy,” a necessary but high-risk strategy for pts with indications for both (e.g., Afib + stent).
- GP IIb/IIIa inhibitors are potent IV “add-on” agents for high-risk PCI procedures.
Irreversible cyclooxygenase inhibitors
Agents
Acetylsalicylic acid (ASA, aspirin)
Mechanism of action
ASA covalently attaches an acetyl group to COX.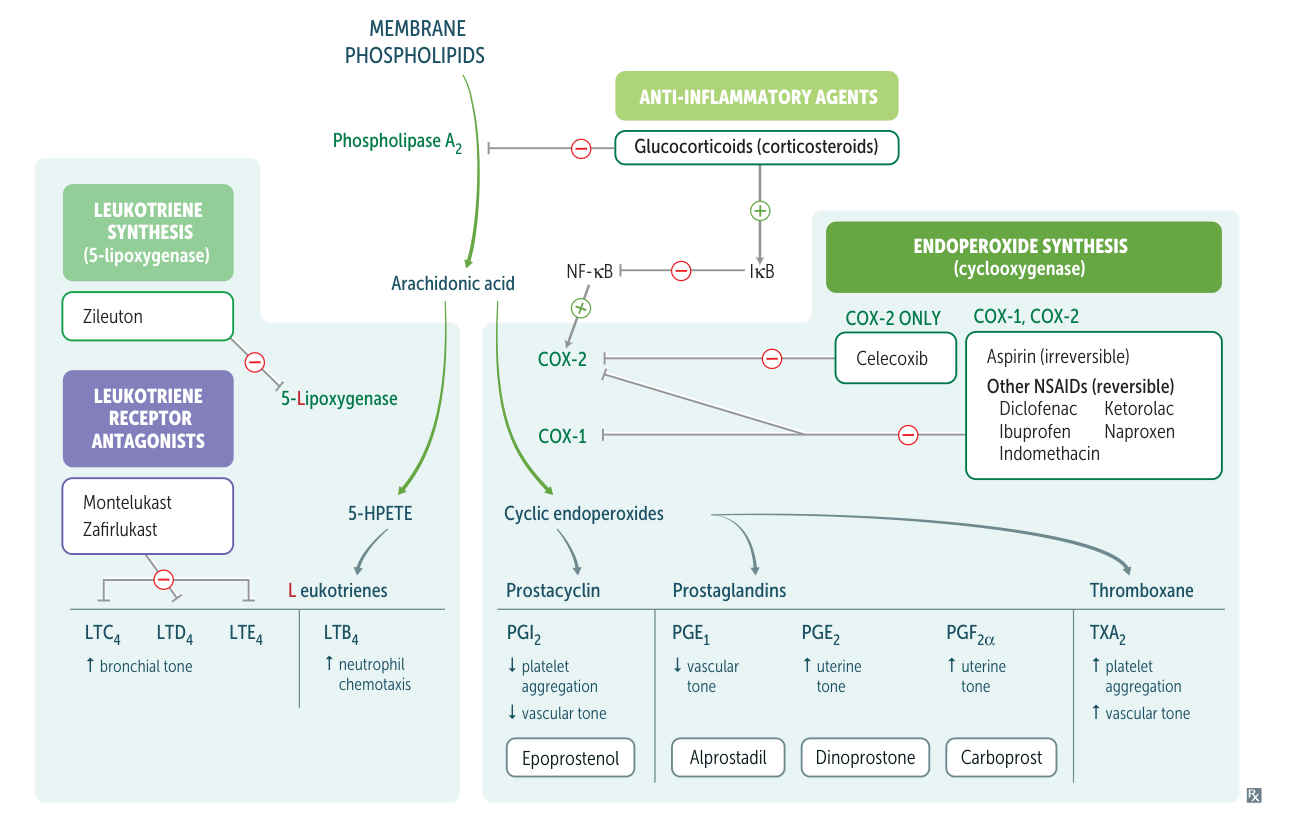
- Irreversible COX-1 inhibition → inhibition of thromboxane (TXA2) synthesis in platelets → inhibition of platelet aggregation (antithrombotic effect)
- Onset of antiplatelet action: within minutes
- Duration of antiplatelet action: 7–10 days
- Irreversible COX-1 and COX-2 inhibition → inhibition of prostacyclin and prostaglandin synthesis → antipyretic, anti-inflammatory, and analgesic effect
- COX-2 is more resistant to inhibition than COX-1. Therefore, higher doses of aspirin are required to achieve the antipyretic, anti-inflammatory, and analgesic effects.
Effects
- Low dose (below 300 mg/day): inhibition of platelet aggregation
- Intermediate dose (300-2400 mg/day): antipyretic and analgesic effect
- High dose (2400-4000 mg/day): antiinflammatory effect
ADP (P2Y12) Receptor Inhibitors
Agents
- Irreversible Antagonists (Thienopyridines):
- Clopidogrel: A prodrug activated by CYP2C19 (genetic variability in efficacy).
- Prasugrel: More potent, more reliable activation than clopidogrel.
- Ticlopidine: Rarely used due to severe side effects.
- Reversible Antagonists:
- Ticagrelor: Not a prodrug, faster onset.
- Cangrelor: IV formulation, very short half-life.
Mechanism of action
- Inhibit platelet aggregation by blocking the P2Y12 ADP receptor on the platelet surface.
- Prevents ADP-mediated activation of the GpIIb/IIIa receptor complex.
Clinical Use
- ACS, especially in combination with aspirin (Dual Antiplatelet Therapy - DAPT).
- Prevention of thrombotic events in patients post-PCI (stenting) or with peripheral arterial disease.
Adverse Effects
- Bleeding (major risk for all).
- Ticlopidine: Neutropenia, agranulocytosis, TTP.
- Prasugrel: Increased bleeding risk vs. clopidogrel; contraindicated in pts with prior stroke/TIA.
- Ticagrelor: Dyspnea, ↑uric acid.
Glycoprotein (Gp) IIb/IIIa Inhibitors
Agents
- Abciximab (Fab region fragments of monoclonal antibodies against glycoprotein IIb/IIIa receptors)
- Eptifibatide
- Tirofiban
Mechanism of action
- Gp IIb/IIIa inhibitors bind to and block glycoprotein IIb/IIIa receptors (fibrinogen receptor) on the surface of activated platelets → prevention of platelets binding to fibrinogen → inhibition of platelet aggregation and thrombus formation
Indication
- Prevention of thrombotic complications in high-risk patients with unstable angina/NSTEMI planned for PCI within 24 hours
Mnemonic
- To remember that ABCiximab targets glycoproteins IIb/IIIa, think ABC rhymes with 123!
- Eptifibatide and tirofiban are fibrinogen receptor blockers.
Phosphodiesterase (PDE) Inhibitors
- Mechanism
- Inhibit phosphodiesterase enzymes, leading to ↑ intracellular cAMP.
- ↑ cAMP impairs platelet aggregation and also causes vasodilation.
- Drugs
- Dipyridamole: Often used with aspirin for secondary stroke prevention. Also used as a pharmacologic cardiac stress agent (vasodilatory properties).
- Cilostazol: A PDE-3 inhibitor.
- Clinical Use
- Dipyridamole: Secondary prevention of ischemic stroke.
- Cilostazol: Symptomatic management of intermittent claudication in peripheral arterial disease (PAD).
- Adverse Effects
- Headache, flushing, hypotension, diarrhea.
- Cilostazol is contraindicated in patients with heart failure.