Epidemiology
- Age
- Primarily affects children (especially between 2–6 years of age)
- Impetigo is highly contagious and can cause epidemics in preschools or schools.
Etiology
- Pathogens: superficial bacterial skin infection
- S. aureus: majority of cases
- Causes both bullous impetigo and nonbullous impetigo
- The blistering in Bullous impetigo is caused by production of exfoliative toxin A, a serine protease that targets desmoglein 1 in the superficial epidermis, by certain strains of S aureus.
- S. pyogenes (GAS): causes nonbullous impetigo
- S. aureus and GAS coinfection may occur
- S. aureus: majority of cases
Pathophysiology
Clinical features
Nonbullous impetigo (~70% of cases)
- Lesions
- Papules that turn into small vesicles surrounded by erythema and/or pustules
- Vesicles and pustules can rupture
- Oozing secretion that dries to form honey-colored crusts that heal without scarring
- May be pruritic (especially pustules) but is rarely painful
- Negative Nikolsky sign
- Papules that turn into small vesicles surrounded by erythema and/or pustules
- Distribution pattern
- Face (most common), especially around the nose and mouth
- Extremities
- Other findings
- Regional lymphadenopathy
Bullous impetigo (~30% of cases)
- Lesions
- Vesicles that grow to form large, flaccid bullae, which go on to rupture and form thin, brown crusts
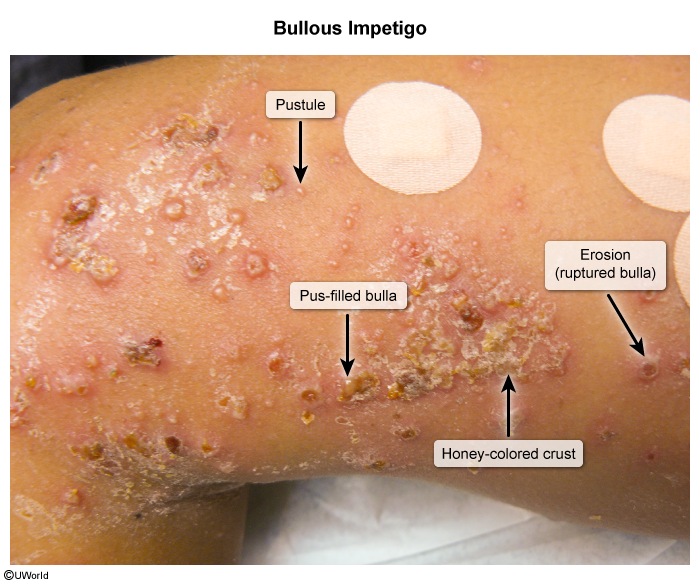
- Negative Nikolsky sign
- Vesicles that grow to form large, flaccid bullae, which go on to rupture and form thin, brown crusts
- Distribution pattern
- Trunk and upper extremities
- Other findings
- Systemic signs (e.g., fever, malaise, weakness) in severe cases
Tip
Impetigo should be suspected in children presenting with honey-colored crusts around the mouth and nose.
Diagnostics
| Characteristic | Pemphigus Vulgaris | Bullous Pemphigoid | Bullous Impetigo |
|---|---|---|---|
| Etiology | Autoimmune disease targeting desmoglein 1 and 3 | Autoimmune disease targeting BP180 and BP230 | Bacterial infection (S. aureus) producing exfoliative toxins |
| Age Group | Middle-aged adults (40-60 years) | Elderly (>65 years) | Children, occasionally adults |
| Level of Skin Separation | Intraepidermal (suprabasal) | Subepidermal | Subcorneal |
| Autoantibodies | Anti-desmoglein 1 and 3 IgG | Anti-BP180 and BP230 IgG | None (bacterial toxin-mediated) |
| Clinical Presentation | • Flaccid blisters that easily rupture • Painful erosions • Mucosal involvement common • Nikolsky sign positive | • Tense bullae on normal or erythematous skin • Less mucosal involvement • Pruritus common • Nikolsky sign negative | • Superficial fragile blisters • Honey-colored crusts • Usually localized • No mucosal involvement |
| Common Sites | Oral mucosa, scalp, face, trunk | Flexural areas, trunk, extremities | Face, extremities, trunk |
| Diagnosis | • Direct immunofluorescence: intercellular IgG • Histology: acantholysis | • Direct immunofluorescence: linear IgG at basement membrane • Histology: subepidermal blister | • Gram stain: gram-positive cocci • Culture: S. aureus |
| Treatment | • Systemic corticosteroids • Steroid-sparing agents (rituximab, azathioprine) • Topical therapy | • Systemic corticosteroids • Steroid-sparing agents • Topical steroids | • Topical antibiotics • Systemic antibiotics if extensive |
| Prognosis | Chronic, potentially life-threatening if untreated | Better than PV, but chronic | Excellent with treatment |
| Complications | • Secondary infections • Fluid/electrolyte imbalance • Malnutrition | • Secondary infections • Side effects of treatment | • Usually self-limited • Rarely systemic infection |