Epidemiology
Etiology
Caused by superantigen toxins from Staphylococcus aureus (TSST-1) or Streptococcus pyogenes (SpeA, SpeC).
- Staphylococcal TSS:
- Source: Often associated with tampon use, nasal packing, or post-surgical wounds.
- Bacteremia: Usually negative; it’s a localized infection with systemic toxin effects.
- Streptococcal TSS (STSS):
- Source: Associated with an invasive infection, typically of the skin/soft tissue (e.g., necrotizing fasciitis, cellulitis).
- Bacteremia: Frequently positive.
- Prognosis: Higher mortality rate than staphylococcal TSS.
Pathophysiology
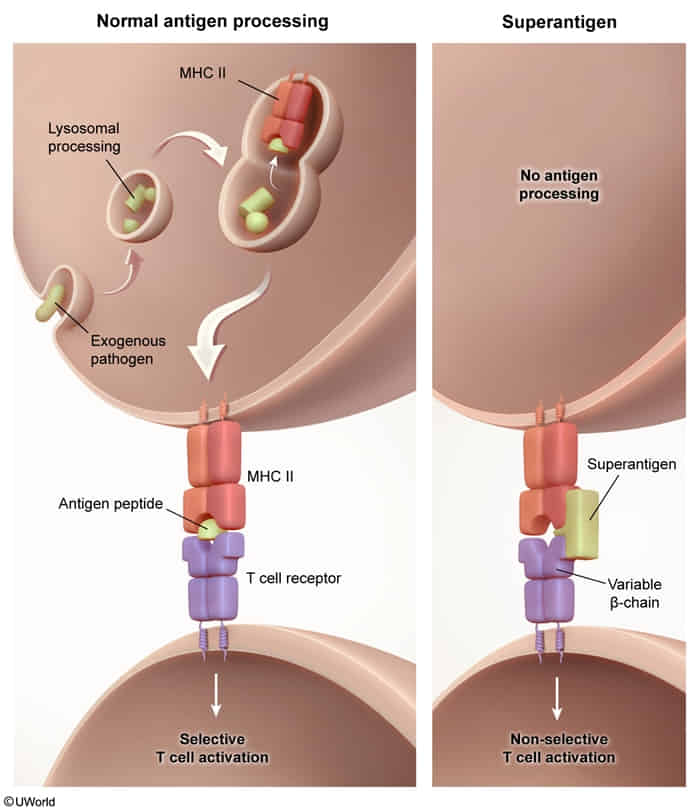
- Superantigen production: Causative organisms (S. pyogenes and S. aureus) produce superantigens
- Superantigen-mediated T-cell activation
- Superantigens bypass processing and presentation by antigen-presenting cells.
- Superantigens directly connect the MHC class II molecule on antigen-presenting cells to the T-cell receptor on T-cells by forming a bridge outside of the normal binding sites → nonspecific T-cell activation → rapid activation of excessive numbers of T cells → massive cytokine release
- SIRS: ↑↑↑ Cytokines → generalized endothelial disruption → capillary leak syndrome → generalized edema → intravascular hypovolemia → organ dysfunction and disseminated intravascular coagulation (DIC)
Clinical features
Prodrome
- Flu-like symptoms: high fever, chills, myalgia, headache, nausea, vomiting, diarrhea
- Dermal rash: more common in menstrual staphylococcal TSS than in nonmenstrual staphylococcal TSS and streptococcal TSS
- Transient erythematous macular (sunburn-like) rash
- Commonly involves the palms and soles
- Typically desquamates 1–2 weeks after onset.
Shock and end-organ dysfunction
- Early: tachycardia, tachypnea, high fever, altered mental status
- Late
- Hypotension
- Delayed capillary refill
- Worsening altered mental status
- Evidence of organ failure