-
Patho/Etiology
- Autosomal Dominant inheritance (most common).
- Mutation in ELANE gene (encodes neutrophil elastase).
- Defective enzyme leads to accumulation of misfolded proteins → accelerated apoptosis of myeloid precursors.
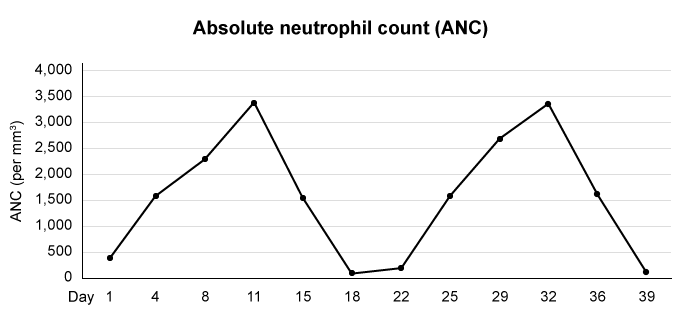
- Characterized by regular, periodic oscillations in Absolute Neutrophil Count (ANC). The cycle is driven by waves of precursor apoptosis followed by compensatory G-CSF surges.
- Classic cycle duration: 21 days (± 3 days).
-
Clinical Presentation
- Usually presents in infancy or early childhood.
- Patients are asymptomatic between episodes. During neutropenic periods, they experience:
- Recurrent fever and malaise.
- Oral manifestations: Aphthous ulcers (mouth sores), gingivitis, pharyngitis. t
- Infections: Recurrent skin infections (cellulitis), sinusitis, and lymphadenopathy.
- Severe infections like pneumonia or sepsis can occur.
-
Diagnosis
- Key diagnostic step: Serial CBC with differential count 2-3 times per week for 6-8 weeks.
- This documents the cyclical pattern of neutropenia, with absolute neutrophil count (ANC) dropping to < 500/µL (often < 200/µL) during nadirs, followed by recovery to normal or near-normal levels.
- Genetic testing for
ELANEgene mutation confirms the diagnosis. - Bone marrow biopsy during a neutropenic episode shows myeloid hypoplasia or maturational arrest at the myelocyte stage.
-
DDx (Differential Diagnosis)
- Severe Congenital Neutropenia (SCN): Also caused by
ELANEmutations, but neutropenia is persistent and severe, not cyclical. SCN carries a higher risk of transformation to AML/MDS. - Autoimmune Neutropenia: Can be associated with other autoimmune conditions (e.g., SLE, Felty syndrome); diagnosed by anti-neutrophil antibodies.
- Drug-induced Neutropenia: Onset is related to a new medication; resolves after discontinuation.
- Viral Infections: (e.g., EBV, Parvovirus B19) can cause transient neutropenia.
- Severe Congenital Neutropenia (SCN): Also caused by
-
Management/Treatment
- First-line: Granulocyte colony-stimulating factor (G-CSF, e.g., filgrastim).
- G-CSF shortens the duration and lessens the severity of neutropenic episodes, reducing the frequency of infections.
- Infections: Prompt treatment with broad-spectrum antibiotics for febrile neutropenia.
- Supportive care: Good oral hygiene is crucial to manage gingivitis and mouth sores.
- Hematopoietic stem cell transplant (HSCT) is rarely needed but can be considered for severe cases unresponsive to G-CSF.
- First-line: Granulocyte colony-stimulating factor (G-CSF, e.g., filgrastim).
-
Key Associations/Complications
- Complications: Severe bacterial infections (e.g., sepsis, pneumonia, necrotizing enterocolitis) are the main risk, especially during neutropenic nadirs.
- Unlike SCN, cyclic neutropenia does not typically carry an increased risk of developing myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML).
- Symptoms may become milder after puberty.