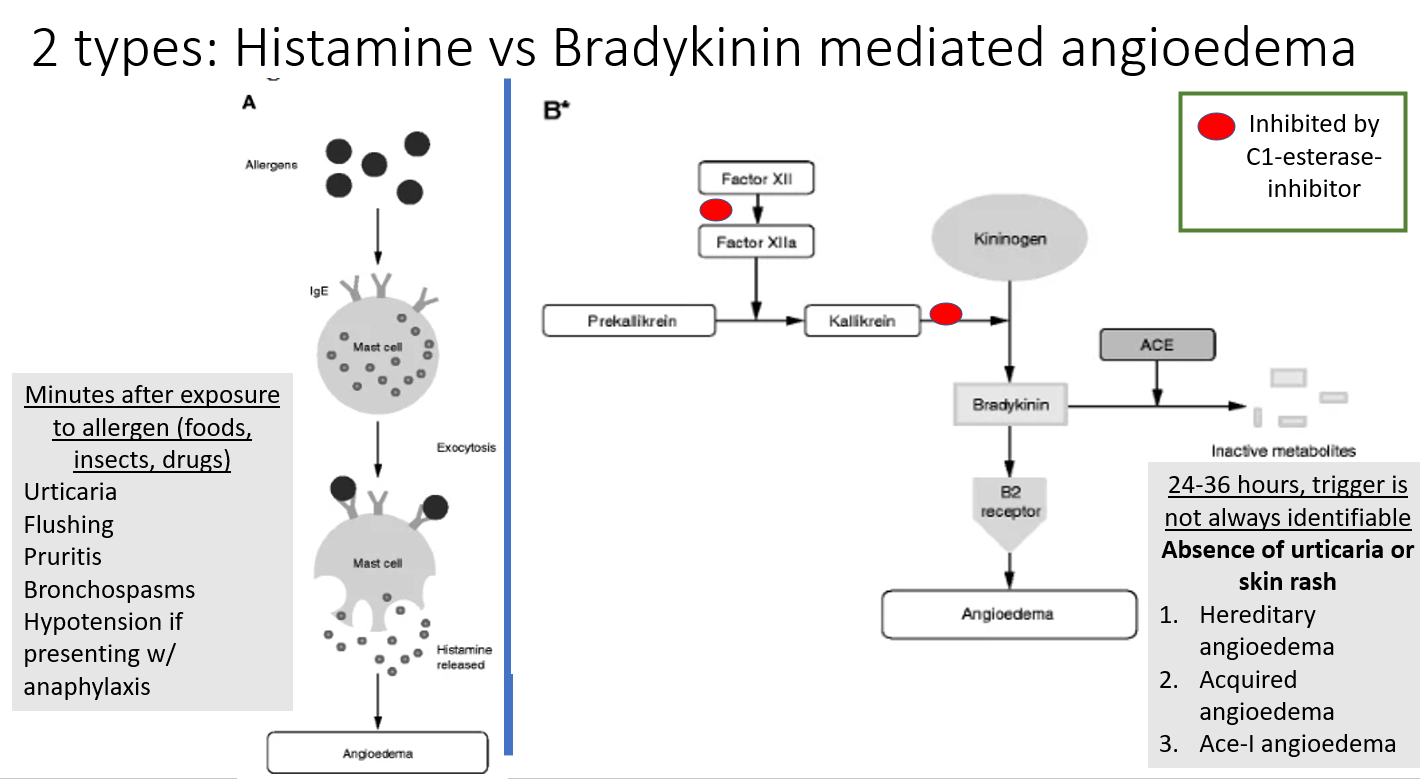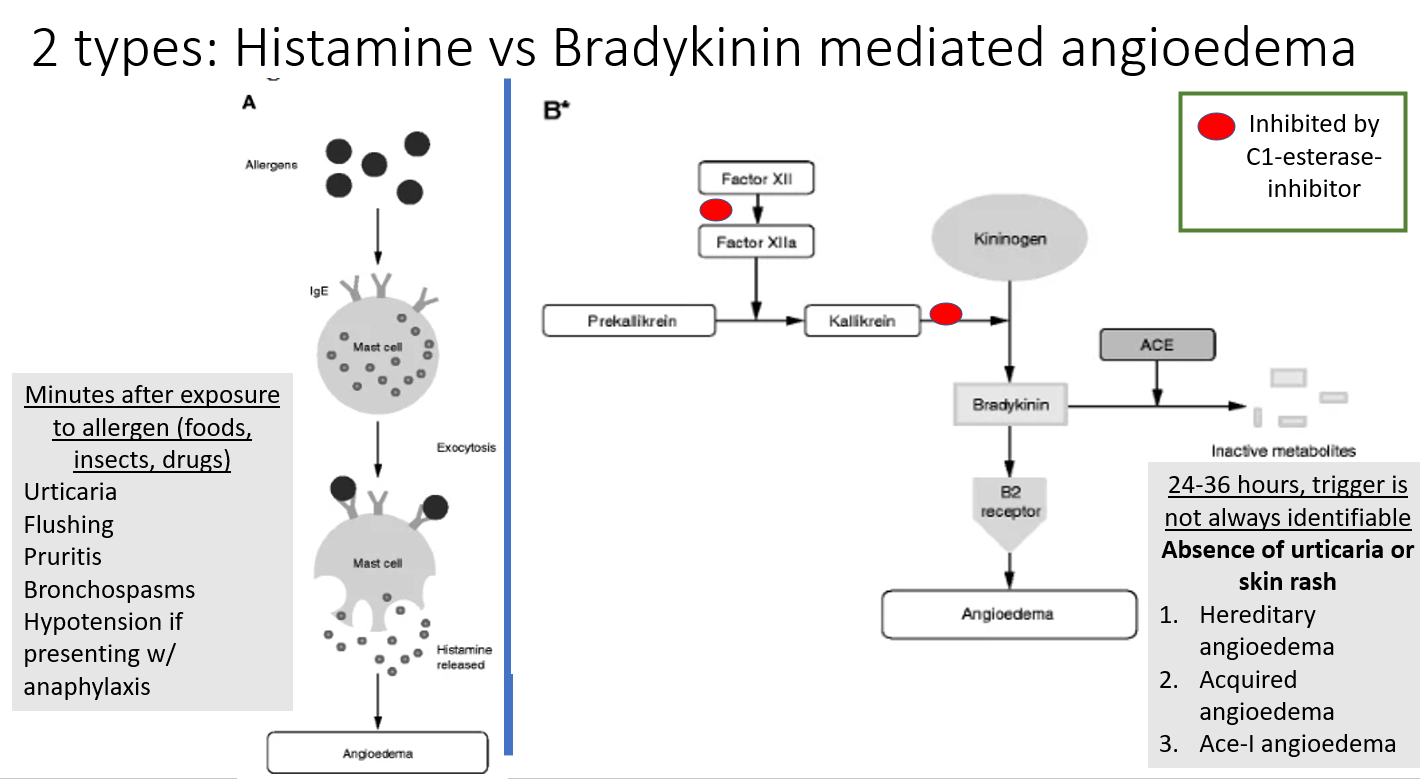
- Mast cell activation
- Excess bradykinin
| Feature | Allergic (Mast Cell) | ACE Inhibitor-Induced | Hereditary Angioedema |
|---|
| Mediator | IgE-mediated type I hypersensitivity → Mast cell degranulation → Histamine release | ACE inhibition prevents breakdown of Bradykinin → Vasodilation & permeability | C1 Esterase Inhibitor Deficiency → Unchecked activation of Kallikrein → ↑ Bradykinin |
| Key Sx | Urticaria + Pruritus | NO urticaria/pruritus | NO urticaria/pruritus + Abd pain |
| Dx | Clinical / ↑ Tryptase | Hx of ACE-I use | ↓ C4 (Screening), ↓ C1-INH |
| Acute Tx | Epinephrine (IM) | Stop drug + Airway | C1-INH concentrate or Icatibant |
| Chronic | Avoid triggers | Switch drug class | Danazol (androgen) |
Kallikrein-Kinin System
- Pathway
- Activation:
- Factor XIIa (Hageman Factor) converts Prekallikrein → Kallikrein.
- Bradykinin Generation:
- Kallikrein cleaves High Molecular Weight (HMW) Kininogen → Bradykinin.
- Degradation:
- Bradykinin is degraded by ACE (Angiotensin Converting Enzyme), also known as Kininase II, and C1 esterase inhibitor.
- Bradykinin Effects
- Vasodilation (via Nitric Oxide & Prostacyclin).
- ACE can ↑ Angiotensin II and ↓ Bradykinin, both contribute to ↑ Blood Pressure
- ↑ Permeability (Edema).
- C1 Esterase Inhibitor can inhibit classical pathway and Kallikrein, both inhibit inflammation.
- Pain.
- High-Yield Associations
- ACE Inhibitors: Block degradation → ↑ Bradykinin → Dry Cough & Angioedema.
- Hereditary Angioedema:
- Deficiency: C1 Esterase Inhibitor (Autosomal Dominant).
- Mechanism: Overactive Kallikrein → ↑ Bradykinin.
- Labs: ↓ C4.
- Contraindication: Do NOT give ACE Inhibitors.