Epidemiology
Etiology
Pathophysiology
DKA
- Primarily a complication of Type 1 Diabetes Mellitus, but can occur in T2DM.
- Caused by a profound insulin deficiency, often precipitated by the “5 I’s”: Infection (most common), Ischemia (MI, CVA), Infarction, Inadequate insulin, and Initial presentation of diabetes.
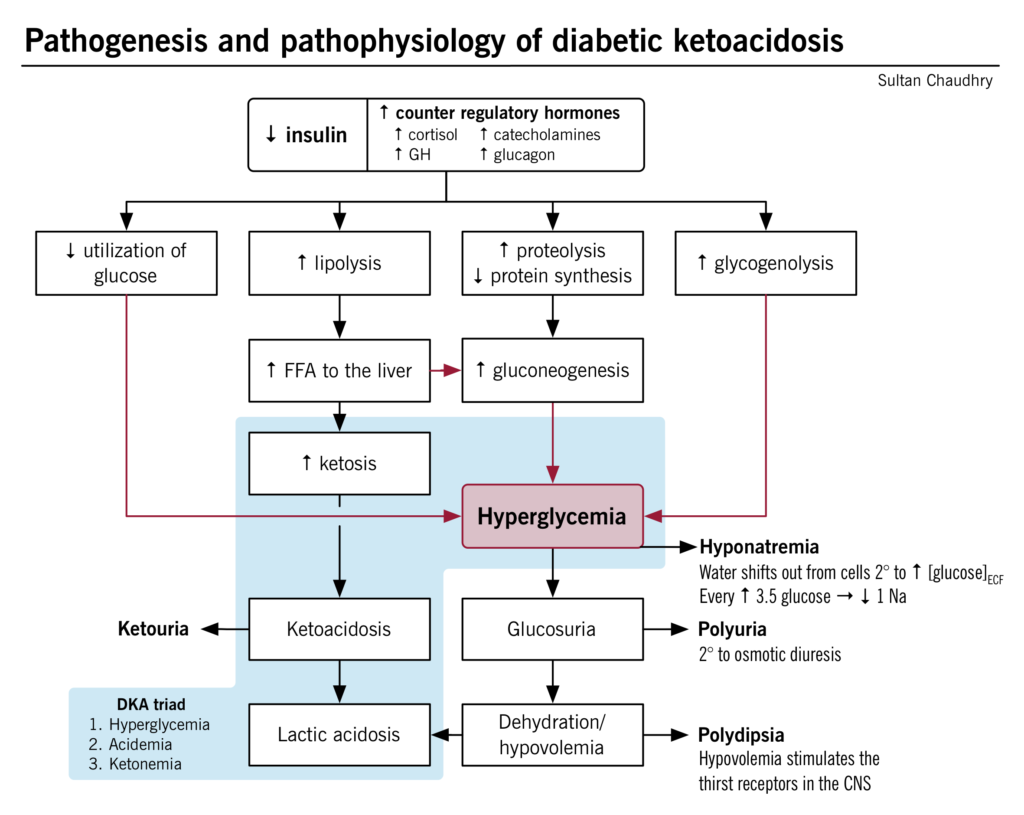
- ↓ Insulin → unopposed counter-regulatory hormones (glucagon, cortisol, catecholamines).
- This hormonal imbalance leads to:
- ↑ Hepatic gluconeogenesis & glycogenolysis → Hyperglycemia.
- ↑ Unrestrained lipolysis → breakdown of triglycerides into free fatty acids.
- The liver converts fatty acids into ketone bodies (β-hydroxybutyrate and acetoacetate), leading to ketosis and metabolic acidosis.
- Hyperglycemia causes osmotic diuresis, leading to severe dehydration and electrolyte loss.
- Insulin deficiency → hyperosmolality → K+ shift out of cells + lack of insulin to promote K+ uptake → intracellular K+ depleted → total body K+ deficit despite normal or even elevated serum K+
Tip
There is a total body potassium deficit in DKA. This becomes important during treatment, when insulin replacement leads to rapid potassium uptake by depleted cells and patients may require potassium replacement.
HHS
- Primarily affects patients with type 2 diabetes
- The pathophysiology of HHS is similar to that of DKA.
- However, in HHS, there are still small amounts of insulin being secreted by the pancreas, and this is sufficient to prevent DKA by suppressing lipolysis and, in turn, ketogenesis.
- HHS is characterized by symptoms of marked dehydration (and loss of electrolytes) due to the predominating hyperglycemia and osmotic diuresis.
Clinical features
Diagnostics
Tip
- DKA is the diagnosis in patients with type 1 diabetes who have hyperglycemia, ketonuria, and high anion gap metabolic acidosis with decreased bicarbonate!
- HHS is the diagnosis in patients with type 2 diabetes who have hyperglycemia and hyperosmolality!
Electrolytes and renal function
- Sodium:
- Hyponatremia is common in both DKA and HHS, due to hypovolemic hyponatremia and hypertonic hyponatremia
- Uncontrolled high blood sugar (hyperglycemia) in DKA acts like a magnet for water.
- This extra sugar in the blood pulls water out of cells, causing them to shrink.
- While the total body water stays the same, the concentration of sodium in the remaining extracellular fluid (outside the cells) gets diluted.
- Always check corrected sodium for hyperglycemia.
- Hyponatremia is common in both DKA and HHS, due to hypovolemic hyponatremia and hypertonic hyponatremia
- Potassium in DKA: normal or elevated (despite a total body deficit)
Treatment
- IV Fluids (IVF) - Highest Priority
- Start immediately with 0.9% Normal Saline (NS), 1-1.5 L in the first hour.
- Once blood glucose (BG) is ~200-250 mg/dL, switch IVF to D5W in 0.45% NS to prevent hypoglycemia and cerebral edema.
- Potassium (K+) - Check Before Insulin
- Crucial: Patients have a total body K+ deficit.
- If K+ is <3.3 mEq/L: HOLD INSULIN. Give K+ first to prevent fatal arrhythmia.
- If K+ is ≥3.3 mEq/L: Give K+ (20-40 mEq/L) along with IVF and insulin.
- Insulin - After Fluids & K+ Check
- Start a continuous IV infusion of Regular Insulin at 0.1 U/kg/hr.
- Goal in DKA: Continue insulin until the anion gap is closed. This is more important than the BG level.