Etiology
ADAMTS13 deficiency
Pathophysiology
Mnemonic
ADAMTS13 deficiency → excess vWF → microthrombus formation → blockage of small vessels → RBC fragmentation (hemolysis) and end-organ damage
TTP is a thrombotic microangiopathy, a condition in which microthrombi form and occlude the microvasculature.
- Autoantibodies or gene mutations → deficiency of ADAMTS13 (a metalloprotease that cleaves von Willebrand factor)
- ↓ Breakdown of vWF multimers → vWF multimers accumulate on endothelial cell surfaces
- Platelet adhesion and microthrombosis
- Microthrombi → fragmentation of RBCs with schistocyte formation → hemolytic anemia
- Arteriolar and capillary microthrombosis → end-organ ischemia and damage, especially in the brain and kidneys (potentially resulting in acute kidney injury or stroke)
Clinical features
- Fever
- Neurological signs and symptoms
- Altered mental status, delirium
- Seizure, focal defects, stroke
- Headache, dizziness
- Low platelet count (i.e. thrombocytopenia)
- Petechiae, purpura
- Mucosal bleeding
- Prolonged bleeding after minor cuts
- Microangiopathic hemolytic anemia
- Fatigue, dyspnea, and pallor
- Jaundice
- Impaired renal function
- Hematuria, proteinuria
Mnemonic
The typical patient is a previously healthy adult presenting with mental status changes, fever, petechiae, fatigue, and pallor. Laboratory tests will then indicate hemolytic anemia and possibly acute kidney injury (AKI). Impaired kidney function may not be present, and only a minority of patients will present with all five clinical findings.
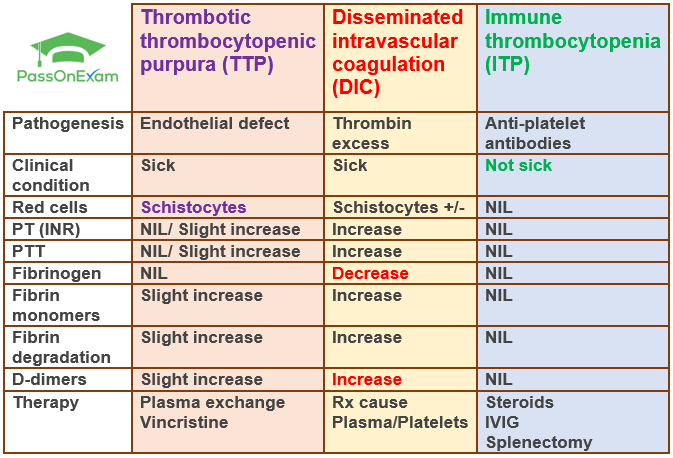
Differential diagnostics
Feature Thrombotic Thrombocytopenic Purpura (TTP) Immune Thrombocytopenia (ITP) Patho ↓ ADAMTS13 activity → Large vWF multimers → microvascular platelet thrombi Anti-platelet (anti-GpIIb/IIIa) Abs → splenic destruction of platelets Presentation Pentad (FAT RN): Fever, Anemia (MAHA), Thrombocytopenia, Renal failure, Neurologic sx (e.g., confusion, stroke). Often acutely ill. Isolated mucocutaneous bleeding (petechiae, purpura, epistaxis). Often asymptomatic. No splenomegaly. Labs MAHA triad: Anemia, Thrombocytopenia, Schistocytes on smear. ↑LDH, ↑Bilirubin, ↓Haptoglobin. Normal PT/PTT. Dx confirmed by ADAMTS13 assay (<10%). Isolated thrombocytopenia (<100,000/µL). Smear may show megathrombocytes. Otherwise normal CBC & smear. Normal PT/PTT. Dx of exclusion. Tx EMERGENT. Plasma exchange (PEX) is first-line & life-saving. Corticosteroids, Rituximab. Platelet transfusion is CONTRAINDICATED (fuels thrombosis). 1st line: Corticosteroids, IVIG. 2nd line: Splenectomy, Rituximab, TPO-RAs (e.g., romiplostim). Observe if plt >30k & no bleeding. Link to original
Treatment
- Medical Emergency: TTP has a high mortality rate (>90%) if untreated. Do not delay treatment while awaiting confirmatory ADAMTS13 results.
- First-Line: Plasma exchange (PEX) / Plasmapheresis is the cornerstone of treatment. It removes autoantibodies and ultra-large vWF multimers while replenishing functional ADAMTS13.
- Immunosuppression:
- Corticosteroids (e.g., prednisone) are given with PEX to suppress autoantibody production.
- Rituximab (anti-CD20 monoclonal antibody) is increasingly used upfront or for refractory/relapsing disease to target B-cells.
- Adjunctive Therapy:
- Caplacizumab: An anti-vWF nanobody that inhibits the interaction between vWF and platelets, leading to a faster rise in platelet count.
- AVOID: Platelet transfusions are generally contraindicated as they can “fuel the fire” and worsen thrombosis, unless there is life-threatening bleeding.