An acquired genetic defect of the hematopoietic stem cell characterized by a triad of hemolytic anemia, pancytopenia, and thrombosis
Epidemiology
Etiology
Pathophysiology
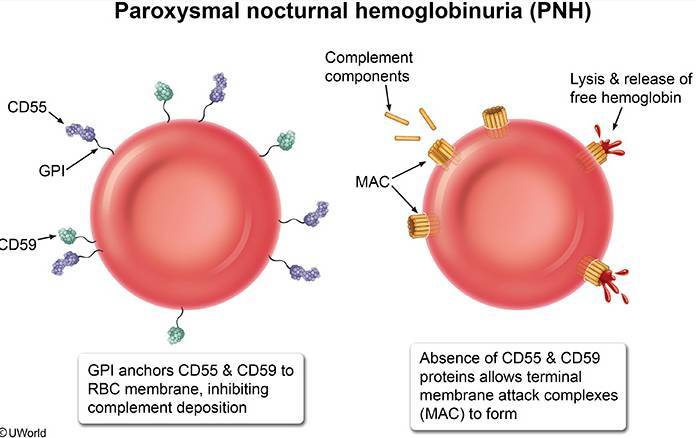
- Physiologically, a membrane-bound glycosylphosphatidylinositol (GPI) anchor protects RBCs against complement-mediated hemolysis.
- Acquired mutation on the PIGA gene located on the X chromosome → GPI anchor loses its protective effect → RBC destruction by complement and reticuloendothelial system → intravascular and extravascular hemolysis
- Hemolysis is often worse at night due to a mild respiratory acidosis during sleep that can enhance complement activation.
- The GPI anchor proteins involved in PNH are:
- CD55/DAF (Decay-accelerating factor)
- CD59/MIRL (Membrane inhibitor of reactive lysis)
- PNH can also occur in patients with aplastic anemia and MDS.
- Autoimmunity to HSCs, causing bone marrow failure → pancytopenia
Mnemonic
MAC inhibitory (CD59) prevents the formation of MAC, which is made up of C5-C9.
Clinical features
- 1. Intravascular Hemolysis:
- Hemoglobinuria: Dark, rust-colored urine, classically in the morning.
- Anemia Sx: Fatigue, dyspnea.
- Jaundice, scleral icterus (from ↑ unconjugated bilirubin).
- 2. Thrombosis:
- Leading cause of death in PNH.
- Occurs in atypical locations: hepatic vein (Budd-Chiari syndrome), portal vein, cerebral veins.
- Both venous and arterial thrombosis.
- Caused by platelet activation and scavenging of nitric oxide (NO) by free plasma hemoglobin, leading to a prothrombotic state.
- 3. Pancytopenia:
- Due to underlying bone marrow dysfunction.
- PNH often arises in the context of or can progress to aplastic anemia.
Diagnostics
- CBC: anemia, thrombocytopenia, and/or pancytopenia ; usually ↑ reticulocytes
- Hemolysis workup: ↓ haptoglobin
- Direct Coombs test: negative
- complement-mediated RBC destruction
- Flow cytometry of peripheral blood (confirmatory test for PNH): can show deficiency of GPI-linked proteins on the surface of RBCs and WBCs (e.g., CD55, CD59)
Treatment
- Indications include severe anemia, thrombosis, severe fatigue, pain crises, and end-organ damage
- First-line treatment: complement inhibition with an anti-C5 antibody (e.g., eculizumab, ravulizumab)
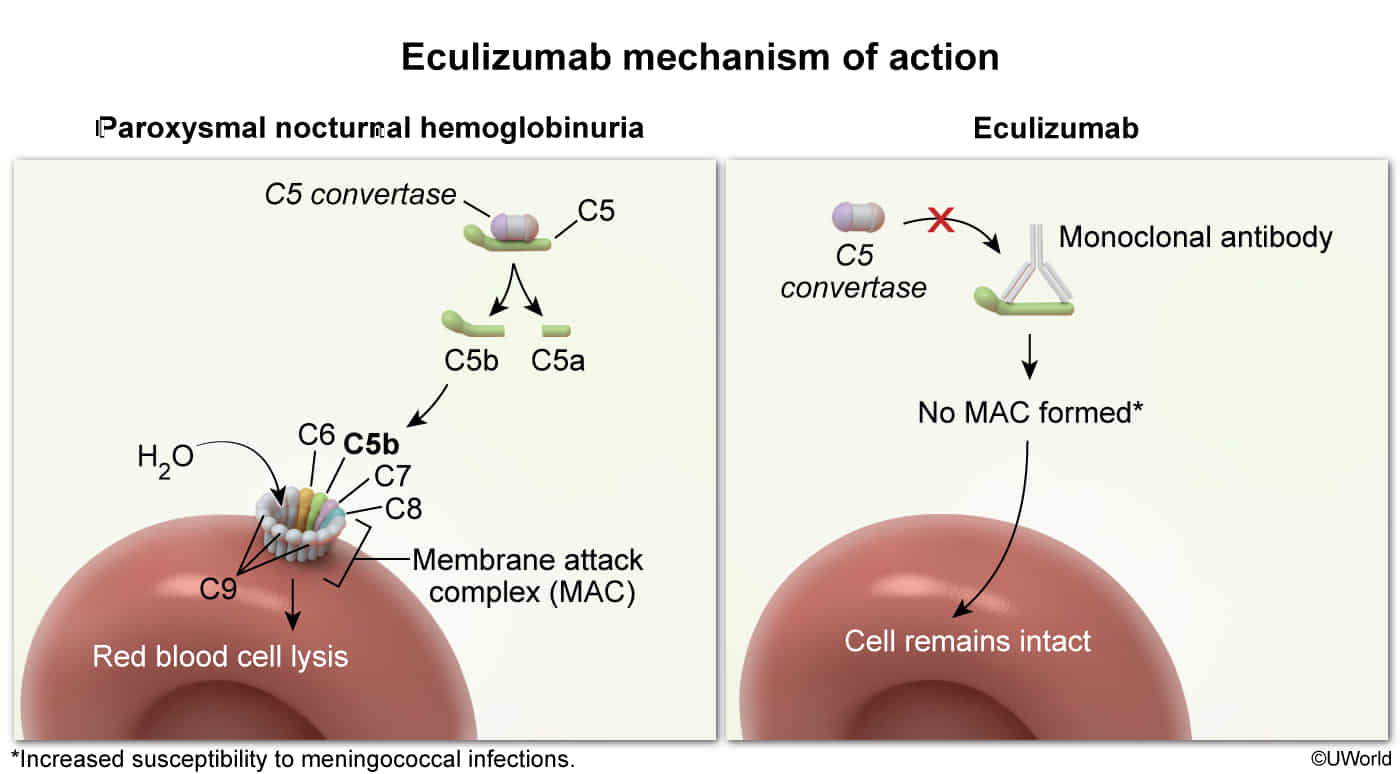
- High Yield Association: Since complement is blocked, patients must receive Meningococcal vaccination (Neisseria meningitidis) prior to therapy due to increased susceptibility to encapsulated bacteria. t