Etiology
- Primary (de novo): Most common, cause is unknown. Risk increases with age (>70 years).
- Secondary (t-MDS): Occurs after exposure to chemotherapy (especially alkylating agents, topoisomerase II inhibitors), radiation, or toxins like benzene.
Pathophysiology
- Clonal hematopoietic stem cell disorders characterized by ineffective hematopoiesis (creates too much ineffective myeloid cells that dies before going to bloodstream), leading to peripheral blood cytopenias despite a typically hypercellular bone marrow. t
- Considered a premalignant condition, with a variable risk of transformation to Acute Myeloid Leukemia (AML).
Classification
French American British (FAB) Classification System
The FAB system divides MDS in to five subtypes based on percentage of blasts in the bone marrow and the peripheral blood. It is now used less frequently than the WHO classification, but is included here as a reference.
| FAB-type | % blasts in blood | % blasts in bone marrow |
|---|---|---|
| RA (Refractory Anemia) | < 1 | < 5 |
| RARS (Refractory Anemia with Ring Sideroblasts | < 1 | < 5 |
| RAEB (Refractory Anemia with Excess Blasts in Transmission) Note: Now called AML (acute myelogenous leukemia) | < 5 | 5 - 20 |
| RAEB-t (Refractory Anemia with Excess Blasts in Transformation) | > 5 | 21 - 30 |
| CMML (chronic myelomonocytic Leukemia) | > 5 | 5 - 20 |
Mnemonic
试着联想记忆: 按照排名分类,人才名单只有<5%,其次是热爱二本的在5%~20%,最后是热爱二本的体育生在20%~30%,所以有Auer小体。其中热爱二本的人也喜欢穿纯棉面料(5%~20%)。
人才名单—RCMD— <5% 热爱二本—RAEB— 5%~20% 热爱二本-体—RAEB-t— 20%~30% 纯棉面料—CMML— 5%~20%
Clinical features
- Often asymptomatic and discovered on routine blood work.
- Symptoms are related to the specific cytopenia(s):
- Anemia (most common): Fatigue, weakness, dyspnea, pallor.
- Neutropenia: Recurrent or severe infections.
- Thrombocytopenia: Petechiae, ecchymoses, epistaxis, or other bleeding.
- Splenomegaly can be seen, particularly in Chronic Myelomonocytic Leukemia (CMML), an MDS/MPN overlap syndrome.
Diagnostics
- CBC:
- Pancytopenia (or uni/bicytopenia).
- Macrocytic anemia (MCV > 100 fL) is a classic finding in elderly pts without B12/folate deficiency.
- Delayed cell division; cell grows too big before dividing.
- Peripheral Blood Smear:
- Dysplastic RBCs (oval macrocytes).
- Defective DNA synthesis shaping the membrane.
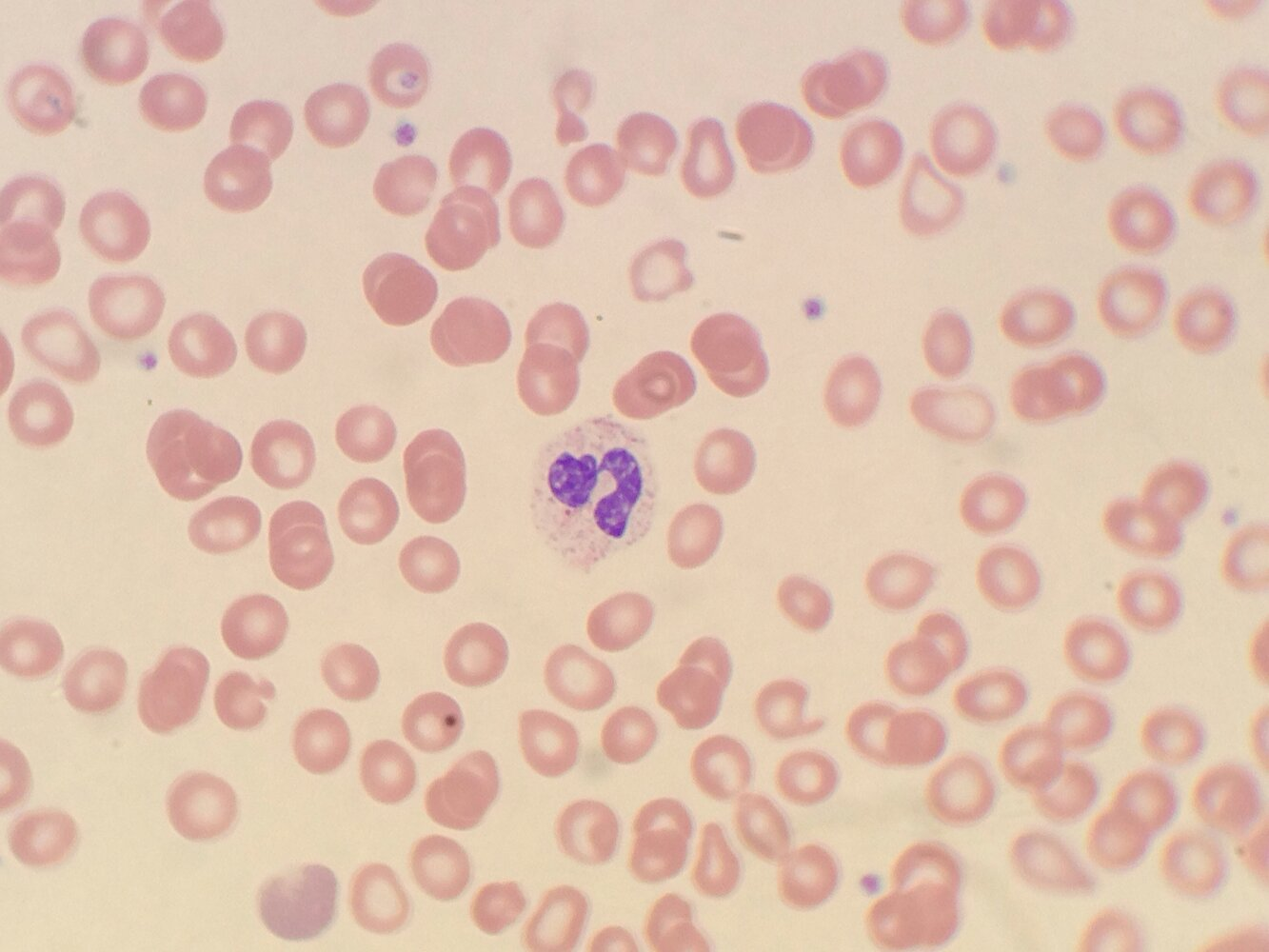
- Pseudo-Pelger-Huët anomaly: Neutrophils with hyposegmented (bilobed) nuclei (“pince-nez” appearance).
- ↓ Lamin B Receptor; failure of nucleus to segment.
- Dysplastic RBCs (oval macrocytes).
- Bone Marrow Biopsy (Definitive Dx):
- Hypercellular marrow (distinguishes from Aplastic Anemia, which is hypocellular/fatty).
- Dysplastic changes in ≥1 cell line.
- Ringed Sideroblasts: Iron-laden mitochondria forming a ring around the nucleus (seen with Prussian blue stain).
- Blast count: < 20% myeloblasts (if > 20%, the diagnosis becomes Acute Myeloid Leukemia [AML]).