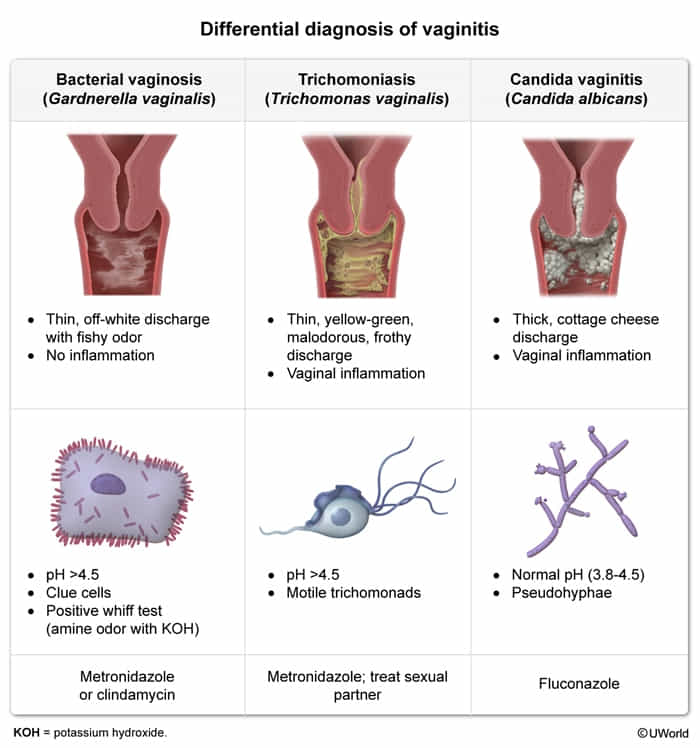
Bacterial vaginosis
Tip
Note this is called “vaginosis” instead of “vaginitis”, because there is no inflammation.
- Epidemiology: most common vaginal infection in women (22–50% of all cases)
- Pathogen: Gardnerella vaginalis (a pleomorphic, gram-variable rod)
- Pathophysiology: lower concentrations of Lactobacillus acidophilus lead to overgrowth of Gardnerella vaginalis and other anaerobes, without vaginal epithelial inflammation due to absent immune response
- Clinical features
- Commonly asymptomatic
- Increased vaginal discharge, usually gray or milky with fishy odor
- Pruritus and pain are uncommon. t
- Diagnostics: diagnosis is confirmed if three of the following Amsel criteria are met
- Clue cells
- Vaginal epithelial cells with a stippled appearance and fuzzy borders due to bacteria adhering to the cell surface
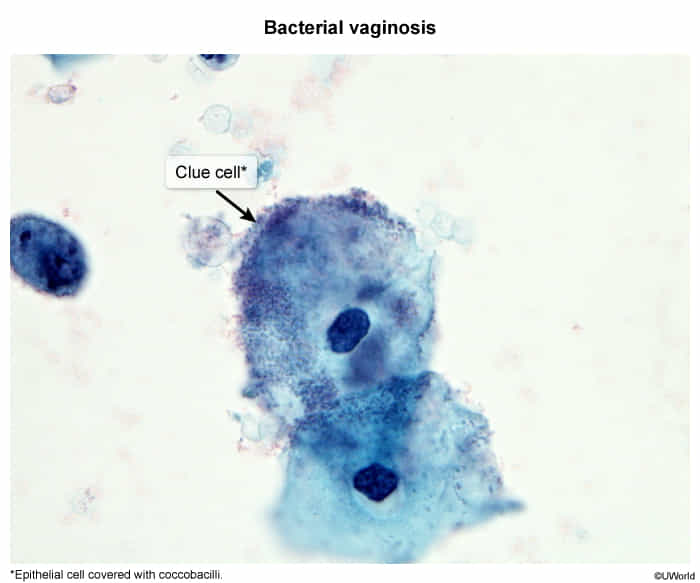
- Identified on a vaginal wet mount preparation
- Vaginal epithelial cells with a stippled appearance and fuzzy borders due to bacteria adhering to the cell surface
- Vaginal pH > 4.5
- Positive amine test (sometimes referred to as the “whiff test”)
- Clue cells
- Treatment
- First-line: metronidazole
- Alternative: clindamycin
Vaginal yeast infection (vulvovaginal candidiasis)
- Epidemiology: second most common cause of vulvovaginitis (17–39% of all cases)
- Pathogen: primarily Candida albicans
- Risk factors
- Pregnancy
- Immunodeficiency, both systemic (e.g., diabetes mellitus, HIV, immunosuppression) and local (e.g., topical corticosteroids)
- Antimicrobial treatment (e.g., after systemic antibiotic treatment)
- Clinical features
- White, crumbly, and sticky vaginal discharge that may appear like cottage cheese t and is typically odorless


- Erythematous vulva and vagina
- Vaginal burning sensation, strong pruritus, dysuria, dyspareunia
- White, crumbly, and sticky vaginal discharge that may appear like cottage cheese t and is typically odorless
Trichomoniasis
- Epidemiology: 4–35% of all cases
- Pathogen: Trichomonas vaginalis
- Clinical features
- Foul-smelling, frothy, yellow-green, purulent discharge
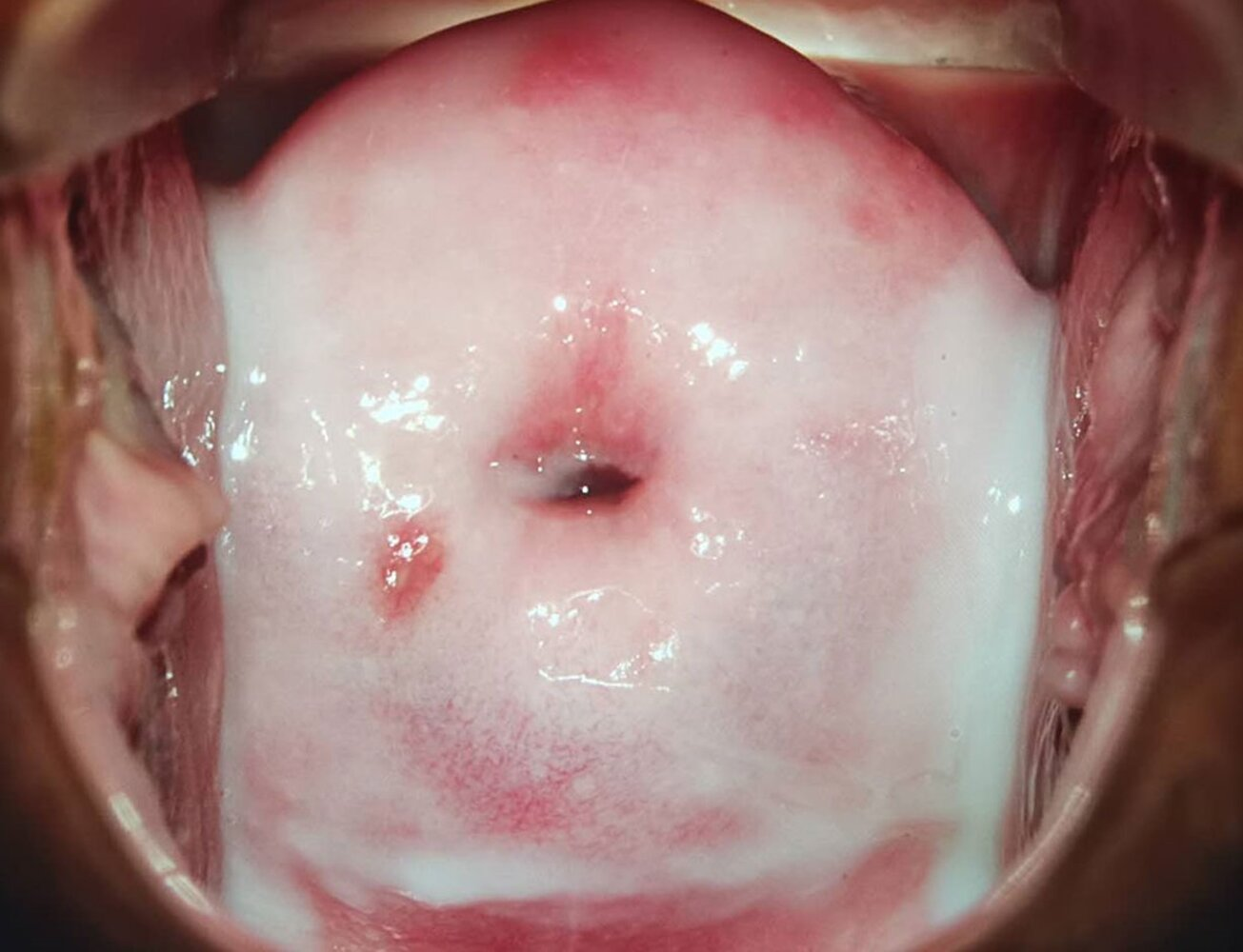
- Vulvovaginal pruritus, burning sensation, dyspareunia, dysuria, strawberry cervix (erythematous mucosa with petechiae)
- Diagnostics
- Saline vaginal wet mount (initial test): motile trophozoites with multiple flagella
- If the wet mount is inconclusive, perform a culture or nucleic acid amplification testing (NAAT)
- pH of vaginal discharge > 4.5
- Routine screening in asymptomatic (nonpregnant and pregnant) patients is not recommended
- Saline vaginal wet mount (initial test): motile trophozoites with multiple flagella