Respiratory muscles
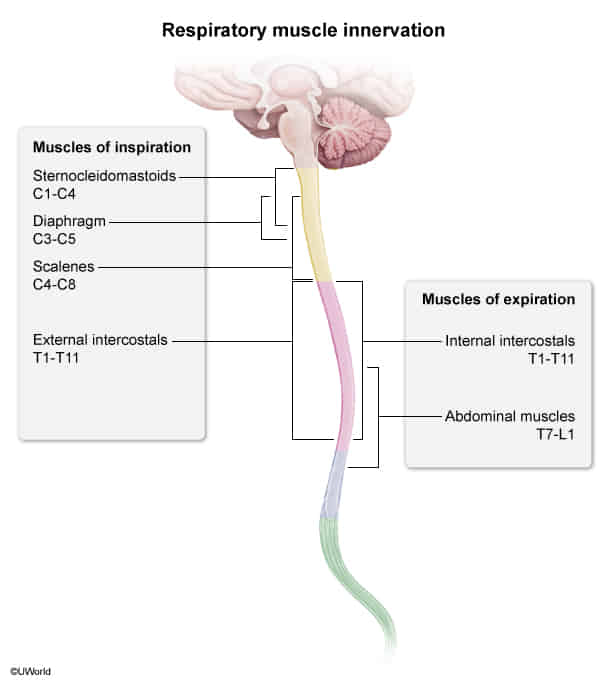
Inspiration
Quiet/Normal Inspiration (Active Process)
- Diaphragm: The primary muscle of inspiration (75% of effort).
- Action: Contracts (flattens/moves inferiorly), increasing the vertical dimension of the thoracic cavity. This creates negative intrathoracic pressure, drawing air into the lungs.
- Innervation: Phrenic nerve (C3, C4, C5 keep the diaphragm alive).
- External Intercostal Muscles:
- Action: Elevate the ribs (“bucket handle” motion), increasing the anteroposterior (A-P) and lateral diameter of the thorax.
- Innervation: Intercostal nerves (T1-T11).
Forced/Active Inspiration
- Involves “accessory muscles” recruited during respiratory distress, exercise, or in chronic pulmonary disease (e.g., COPD).
- Accessory Muscles:
- Sternocleidomastoid (SCM): Elevates the sternum.
- Scalene Muscles (Anterior, Middle, Posterior): Elevate the upper ribs.
- Pectoralis Major & Minor: Elevate the chest/ribs.
- Serratus Anterior & Latissimus Dorsi: Can assist in elevating the ribs.
Expiration
Quiet/Normal Expiration (Passive Process)
- No muscle contraction is required.
- Driven by the elastic recoil of the lungs and chest wall after the diaphragm and external intercostals relax.
Forced/Active Expiration (Active Process)
- Used during exertion (e.g., exercise, coughing, sneezing) or in diseases with airway obstruction (e.g., asthma, COPD).
- Muscles:
- Abdominal Muscles (most important):
- Rectus abdominis, internal/external obliques, transversus abdominis.
- Action: Increase intra-abdominal pressure, pushing the diaphragm up and decreasing thoracic volume.
- Internal Intercostal Muscles:
- Action: Depress the ribs, decreasing the A-P and lateral diameter of the thorax.
- Abdominal Muscles (most important):
Gas exchange
Types of gas exchange
- Perfusion-limited gas exchange: Gas exchange is limited by the rate of blood flow through the pulmonary capillaries.
- Gases (e.g., O2, CO2, N2O) can diffuse freely across the blood-air barrier.
- The concentration of gases in the plasma will become equal to the concentration in the alveoli before the blood reaches the end of the capillary.
- An increase in blood flow causes an increase in gas exchange .
- Occurrence: under normal conditions (i.e., at rest)
- Diffusion-limited gas exchange: Gas exchange is limited by the diffusion rate of the gas (e.g., O2, CO) across the blood-air barrier.
- The gas concentration in the plasma will not be in equilibrium at the end of the capillary.
- Occurrence
- Strenuous exercise
- In certain pathological conditions that affect the blood-air barrier (e.g., emphysema, lung fibrosis)
Tip
Under normal physiological conditions, O2 transport is generally perfusion-limited, while it can become diffusion-limited in pathological states or during intense exercise.
Lung and chest wall compliance (pressure-volume curve)
Concepts
- Elastic Recoil: Lungs’ tendency to passively collapse after being stretched. Driven by elastin & alveolar surface tension.
- As lung volume ↑, Elastic Recoil ↑
- Lung Compliance (CL): Measure of lung stretch (ΔV/ΔP). How easily the lungs inflate. Inversely related to elastic recoil.
- Compliance is highest at mid-range volumes (FRC) and lowest at the extremes (RV and TLC).
- Surfactant: Secreted by Type II pneumocytes. Decreases alveolar surface tension, which increases compliance and prevents alveolar collapse (atelectasis). Deficiency causes Neonatal Respiratory Distress Syndrome (NRDS).
- Functional Residual Capacity (FRC): Volume in lungs after normal, passive exhalation. This is the equilibrium point where the inward pull of the lungs (elastic recoil) is balanced by the outward spring of the chest wall.
- Y-axis: Volume. This represents the volume of air in the lungs.
- X-axis: Recoil Pressure. This represents the pressure exerted by the lungs and chest wall trying to return to their resting state. Note that recoil pressure is presented with negative and positive values.
- Positive values of recoil pressure indicate a “collapsing force.” This means the lungs want to collapse inward (due to their elastic recoil and surface tension).
- Negative values of recoil pressure indicate an “expanding force.” This means the chest wall wants to spring outward.
Drawing 2025-04-17 11.09.49.excalidraw
⚠ Switch to EXCALIDRAW VIEW in the MORE OPTIONS menu of this document. ⚠ You can decompress Drawing data with the command palette: ‘Decompress current Excalidraw file’. For more info check in plugin settings under ‘Saving’
Excalidraw Data
Text Elements
② ↑ Lung compliance & ↑↑↑ Chest wall compliance
① 0 Lung compliance & (-Inf) Chest wall compliance
③ + Lung compliance = - Chest wall compliance Lung at rest
Embedded Files
a971bd3f45374f562d1f6e3a9a4bd30da9075166: Pasted Image 20250417111043_161.png
Link to original
Anatomy
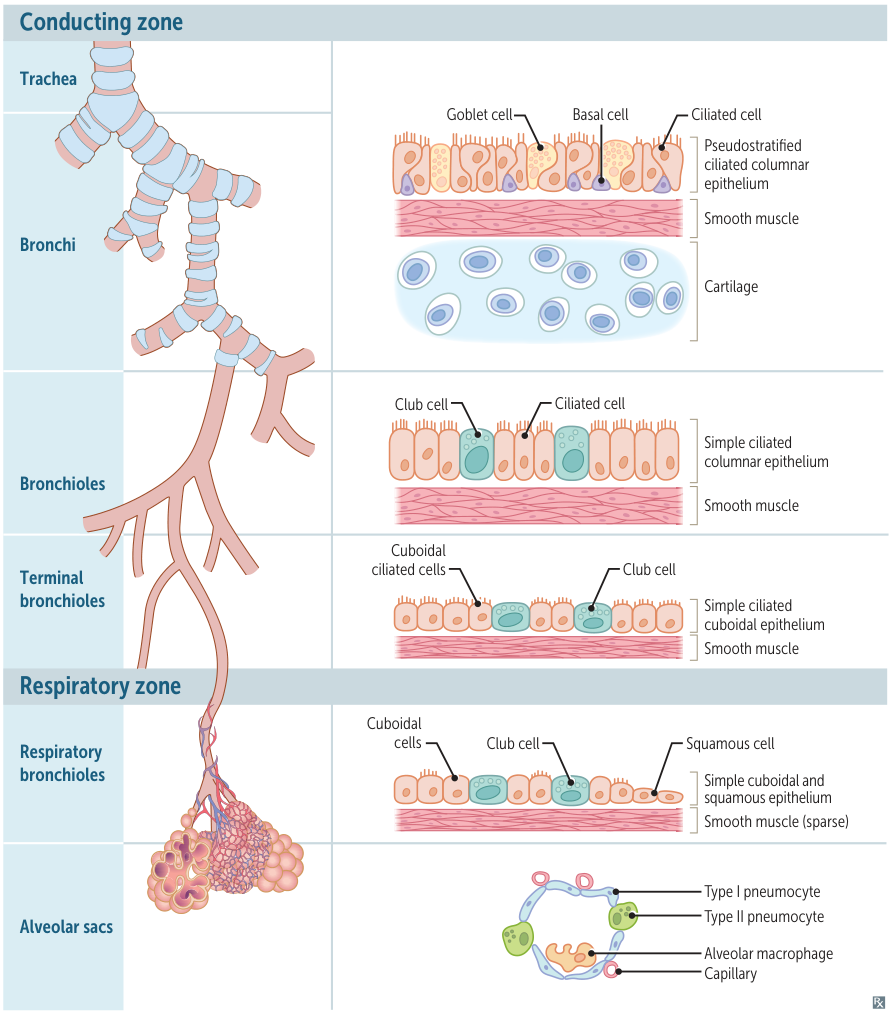 The overall trend in the respiratory tract is for the epithelium to become progressively thinner as it approaches the alveoli (where it’s extremely thin simple squamous epithelium) to facilitate gas diffusion.
The overall trend in the respiratory tract is for the epithelium to become progressively thinner as it approaches the alveoli (where it’s extremely thin simple squamous epithelium) to facilitate gas diffusion.
I. Conducting Zone (Anatomic Dead Space)
-
Function: Warms, humidifies, and filters air. No gas exchange.
-
Epithelium Trend: Pseudostratified ciliated columnar → simple columnar → simple cuboidal.
-
Structural Trend: Cartilage & goblet cells decrease; smooth muscle becomes more prominent.
-
Trachea & Bronchi:
- Epi: Pseudostratified ciliated columnar with goblet cells (mucus).
- Structure: Supported by cartilage (C-rings in trachea, plates in bronchi) and contain submucosal glands. Mucociliary escalator clears debris.
-
Bronchioles:
- Epi: Simple columnar to cuboidal. Goblet cells are replaced by Club (Clara) cells.
- Club (Clara) Cells: Secrete surfactant components & act as progenitor cells.
- Structure: No cartilage, no glands. Prominent smooth muscle layer (pathology in asthma).
-
Terminal Bronchioles: Smallest airways of the conducting zone.
II. Respiratory Zone (Gas Exchange)
-
Respiratory Bronchioles:
- Cuboidal epithelium with Club cells.
- First site of gas exchange; walls have scattered alveoli.
-
Alveoli:
- Type I Pneumocytes: (95% surface area) Thin, squamous cells forming the barrier for gas exchange.
- Type II Pneumocytes: (5% surface area) Cuboidal cells that produce surfactant (dipalmitoylphosphatidylcholine) to prevent alveolar collapse and act as stem cells for both Type I & II cells.
- Alveolar Macrophages (Dust Cells): Phagocytose debris. (Become “hemosiderin-laden macrophages” in HF or pulmonary hemorrhage).
Pneumocytes
- Type I pneumocytes: thin squamous cells that line the alveoli that allow for transcellular gas exchange
- Comprise 95% of the total alveolar area
- Connected to each other by tight junctions
- Form the blood-air barrier, together with the endothelial cells of the capillaries and the basement membrane between the two cells.
- Type II pneumocytes: cuboidal alveolar cells
- Comprise 5% of the total alveolar area, but 60% of total number of cells
- Surfactant formation: Type II pneumocytes contain lamellar bodies, which secrete surfactant (surface-activating lipoprotein complex).
- Surfactant is mainly composed of the phospholipids dipalmitoylphosphatidylcholine (DPPC or lecithin) and phosphatidylglycerol.
- It reduces alveolar surface tension and thereby prevents the alveoli from collapsing.
- Imagine a bubble. The film of the bubble has surface tension, which tends to make the bubble as small as possible. Now, imagine adding a special substance (like surfactant) to the bubble’s film. This substance has one end that likes water and one end that doesn’t. The water-liking ends stick into the film, while the other ends stick out. This disrupts the pull between the water molecules in the film, reducing the surface tension and making it easier for the bubble (alveolus) to stay inflated.
- Lung regeneration and repair: Type II pneumocytes can proliferate to replace type I or type II pneumocytes following lung damage.
Respiratory adaptation
Respiratory adaptation to exercise
- ↑ O2 consumption and ↑ CO2 production lead to ↑ depth and rate of ventilation (hyperventilation).
- ↑ Venous CO2 and ↓ venous O2
- PaCO2 and PaO2 remain normal despite hyperventilation.
- ↑ HR and ↑ SV → ↑ cardiac output → ↑ pulmonary blood flow
- ↓ Arterial pH (due to lactic acidosis)
- Rightward shift of the oxygen dissociation curve
- Oxygen diffusion becomes diffusion-limited (in resting state it is perfusion-limited).
- ↑ V/Q ratio (from base to apex) → V/Q ratio is more evenly distributed throughout the lung during exercise than at rest
Respiratory adaptation to high altitude
Decreased atmospheric oxygen (PiO2) at high altitudes triggers various adaptation mechanisms in the respiratory system. Insufficient adaptation to the high altitude results in altitude sickness.
- ↓ PaO2 → ↑ ventilation rate (stimulated by hypoxemia) → ↓ PaCO2 and ↑ arterial pH (respiratory alkalosis)
- ↑ Renal HCO3− excretion (to compensate for respiratory alkalosis)
- ↑ Pulmonary vascular resistance (Euler-Liljestrand reflex): chronic hypoxia → pulmonary vasoconstriction → pulmonary hypertension → right ventricular hypertrophy
- ↑ Hb and hematocrit (due to chronic hypoxia triggering ↑ erythropoietin levels)
- ↑ 2,3-BPG concentration → ↓ Hb affinity to O2 → rightward shift of the oxygen dissociation curve
- ↑ Number of mitochondria in cells
Perfusion
Pulmonary vascular resistance
- Definition
- Resistance to blood flow through the pulmonary circulation
- Formula: PVR = (mPAP - PCWP) / CO
- mPAP = mean pulmonary artery pressure
- PCWP = pulmonary capillary wedge pressure (≈ left atrial pressure)
- CO = cardiac output
- Normal: 0.25-1.6 Wood units (or 20-130 dyne·s·cm⁻⁵)
Hypoxic Pulmonary Vasoconstriction (HPV)
- Pathophysiology/Etiology
- Unique Response: Unlike systemic circulation which vasodilates in response to hypoxia, the pulmonary arteries constrict. This is a fundamental physiological reflex also known as the Euler-Liljestrand mechanism.
- Mechanism: Alveolar hypoxia is sensed by pulmonary artery smooth muscle cells (PASMCs). This leads to inhibition of voltage-gated potassium (K+) channels in the PASMC membrane. The decreased K+ efflux causes cell membrane depolarization, which activates voltage-gated calcium (Ca2+) channels. The subsequent influx of Ca2+ triggers smooth muscle contraction and vasoconstriction.
- Physiological Function
- V/Q Matching: The primary role of HPV is to optimize ventilation/perfusion (V/Q) matching. It diverts blood flow away from poorly ventilated (hypoxic) areas of the lung and towards well-ventilated areas. This minimizes shunting of deoxygenated blood and maximizes systemic arterial oxygenation.
- Fetal Circulation: In the non-ventilated fetal lungs, diffuse HPV is crucial. It increases pulmonary vascular resistance, shunting blood from the pulmonary artery through the ductus arteriosus to the systemic circulation.
- Clinical Relevance & Key Associations
- Beneficial in Localized Hypoxia: HPV is protective in conditions like pneumonia, atelectasis, or one-lung anesthesia during thoracic surgery. By constricting vessels in the non-ventilated lung, it maintains oxygenation and reduces shunting.
- Detrimental in Global Hypoxia: In conditions of widespread alveolar hypoxia, such as high altitude or chronic obstructive pulmonary disease (COPD), generalized HPV occurs.
- This leads to a diffuse increase in pulmonary vascular resistance, causing pulmonary hypertension (PH).
- Chronic PH can lead to right ventricular hypertrophy (cor pulmonale) and right heart failure.
- High-Altitude Pulmonary Edema (HAPE): An exaggerated HPV response at high altitude can lead to a rapid and severe increase in pulmonary artery pressure, causing HAPE.
- Inhibition of HPV: Certain factors can inhibit the HPV response, which can worsen V/Q mismatch and lead to hypoxemia. These include:
- Inhaled anesthetics (in a dose-dependent manner)
- Vasodilator drugs (e.g., calcium channel blockers, nitric oxide)
- Acidosis or alkalosis
- Sepsis
Regulation of respiration
Central Control
- Medullary Centers
- Dorsal Respiratory Group (DRG): Primary inspiratory center
- Ventral Respiratory Group (VRG): Forced expiration/inspiration
- Pre-Bötzinger Complex: Respiratory pacemaker
- Pontine Centers
- Pneumotaxic: Inhibits inspiration → ↑ RR
- Apneustic: Stimulates inspiration
Chemoreceptors
- Central (Medulla)
- Sense ↑ PCO2 (via ↑ H+ in CSF)
- Primary controller of minute-to-minute ventilation
- Peripheral (Carotid/Aortic Bodies)
- Sense ↓ PO2 (primary), ↑ PCO2, ↑ H+
- Only sensors for hypoxemia
- Respond when PaO2 <60 mmHg
- Important in chronic hypercapnia (central receptors adapt)
Mechanoreceptors
- Stretch Receptors: Hering-Breuer reflex - prevent overinflation
- Irritant Receptors: Trigger cough, bronchoconstriction
- J-Receptors: Respond to edema/emboli → rapid shallow breathing
Clinical Pearls
- Chronic COPD: Central receptors adapt → hypoxic drive via peripheral receptors (caution with high-flow O2)
- Opioid OD: Suppresses medullary centers → respiratory depression
- Ondine’s Curse: Loss of automatic control