Etiology
- Most common: Deep vein thrombosis
- Causes of nonthrombotic embolism
- Fat embolism
- Air embolism
- Amniotic fluid embolism
- Bacterial embolism
- Patients with intravenous drug use are at increased risk of developing tricuspid valve endocarditis, giving rise to septic pulmonary emboli
- Others: pulmonary tumor embolism, pulmonary cement embolism
Tip
Up to 30% of cases may present with no apparent risk factors (eg, hypercoagulability).
Pathophysiology
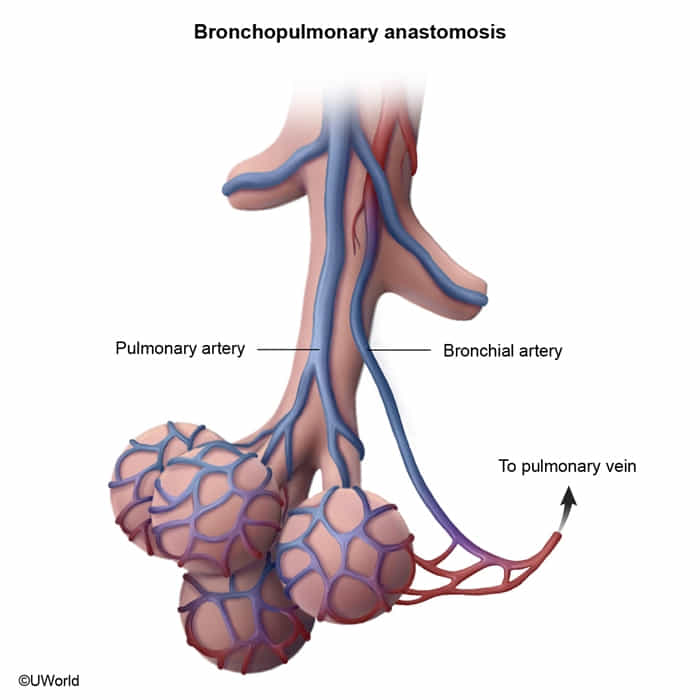
- Dual Blood Supply: The lungs are supplied by two circulations:
- Pulmonary Arteries: Low-pressure system carrying deoxygenated blood from the RV for gas exchange.
- Bronchial Arteries: High-pressure system arising from the aorta; supplies oxygenated blood to the lung parenchyma (bronchi, connective tissue).
- Pulmonary Infarction:
- Due to the dual blood supply, PE does not always cause pulmonary infarction (tissue death). The bronchial circulation can often sustain the lung tissue.
- Infarction is more likely to occur if the bronchial circulation is compromised (e.g., in left-sided heart failure) or if the embolus is very peripheral.
- When it occurs, it’s typically a hemorrhagic (red) infarct because some blood from the bronchial circulation still leaks into the necrotic area.
- Clinically, it presents with pleuritic chest pain and hemoptysis. Radiologically, it may appear as a wedge-shaped infiltrate (Hampton’s Hump).
Clinical features
- Common features of PE
- Acute onset of symptoms
- Dyspnea (> 75% of cases)
- Tachycardia and tachypnea (up to 50% of cases)
- Sudden pleuritic chest pain (∼ 20% of cases)
- Cough and hemoptysis
- Associated features of DVT: e.g., unilaterally painful leg swelling
- Features of massive PE (e.g., due to a saddle thrombus)
- Presyncope or syncope
- Jugular venous distension and Kussmaul sign
- RV pressure overload
- Hypotension and obstructive shock
- Circulatory collapse
Diagnostics
Confirmatory imaging
CT pulmonary angiography (CTPA)
CTPA is the preferred test for the diagnosis of acute PE.
- Findings
- Direct finding of PE: intraluminal filling defects of pulmonary arteries
- Pulmonary infarct: opacity with consolidated border; may be accompanied by pleural effusion
Severity assessment
ECG
ECG changes may be due to right ventricular strain and pressure overload. Most common findings
- T-wave inversions or flattening
- Sinus tachycardia
- Normal ECG
- S1Q3T3 pattern (neither sensitive nor specific)
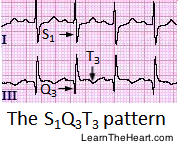 Predictors of adverse outcomes: See “High-risk ECG findings in PE.”
Other ECG findings in PE: sinus bradycardia (< 60/min); uncommon)
Predictors of adverse outcomes: See “High-risk ECG findings in PE.”
Other ECG findings in PE: sinus bradycardia (< 60/min); uncommon)
Treatment
Reperfusion therapy
- Indications
- Massive PE (hemodynamic instability and/or right heart failure) with a low bleeding risk
- Recombinant tissue plasminogen activator (tPA), e.g., alteplase (preferred)
- Endothelial-derived TPA is limited primarily to the bronchial circulation, and spontaneous recanalization of the pulmonary artery is a slow process.