-
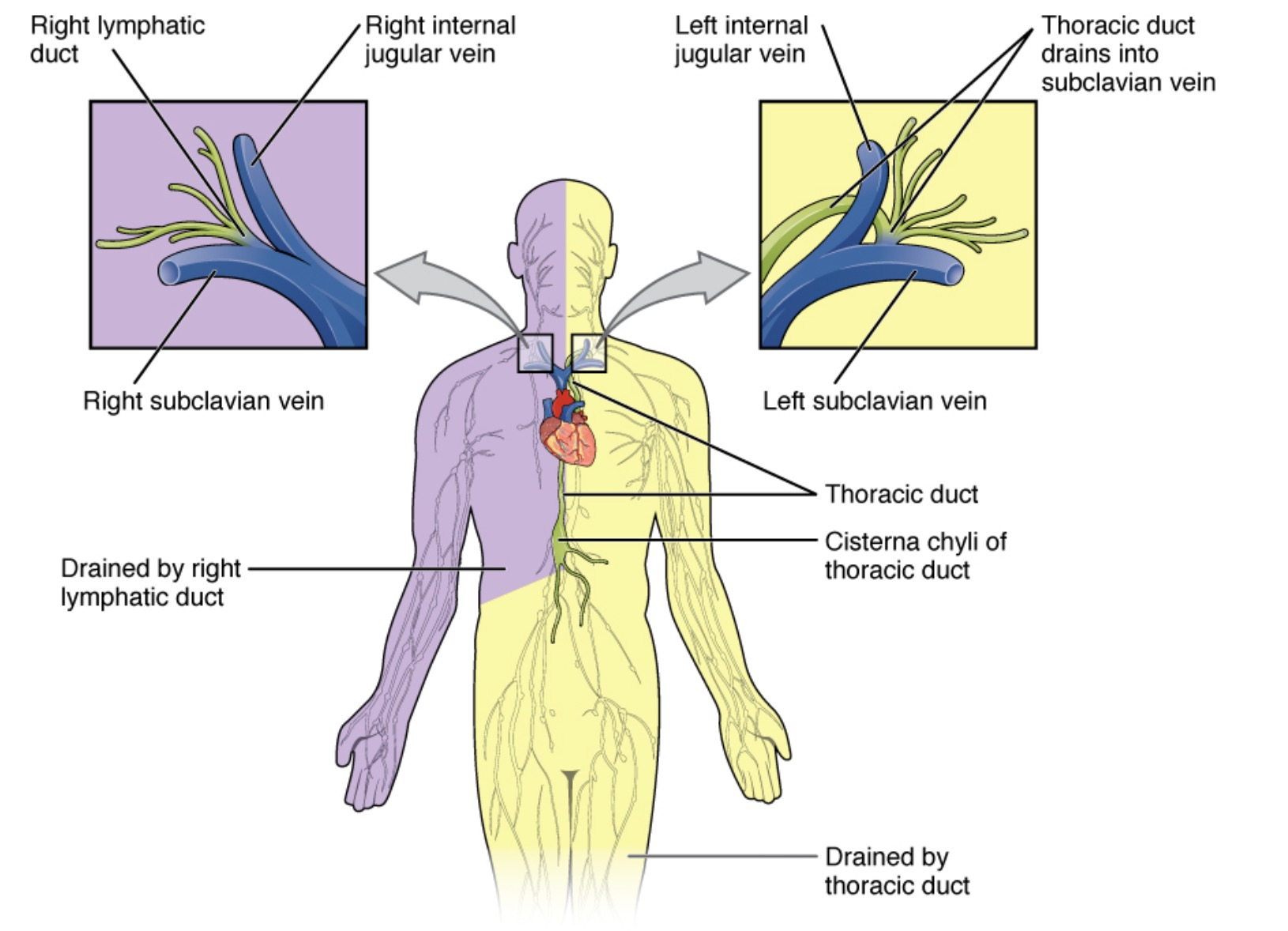
Patho/Etiology: Accumulation of chyle (lymphatic fluid from the intestines) in the pleural space due to disruption or obstruction of the thoracic duct.
- Traumatic: Most common overall cause. Often iatrogenic, secondary to thoracic surgery (e.g., esophagectomy, cardiac surgery) or chest trauma.
- Non-traumatic: Malignancy is the most frequent non-traumatic cause, especially lymphoma. Other causes include infections (e.g., TB, filariasis), sarcoidosis, cirrhosis, and superior vena cava (SVC) thrombosis.
- Traumatic: Most common overall cause. Often iatrogenic, secondary to thoracic surgery (e.g., esophagectomy, cardiac surgery) or chest trauma.
-
Clinical Presentation: Symptoms relate to the size and rate of fluid accumulation.
- Progressive dyspnea is the most common symptom.
- Cough, chest pressure.
- Fever and sharp chest pain are typically absent.
- Signs of pleural effusion on exam: decreased breath sounds, dullness to percussion.
- Post-traumatic chylothorax may present up to 10 days after the initial injury.
-
Diagnosis:
- Thoracentesis (Gold Std): Pleural fluid analysis is key.
- Appearance: Milky, opalescent fluid is classic but only seen in about half of cases; can be serous or serosanguineous, especially in fasting patients.
- Biochemistry: Definitive diagnosis relies on lipid analysis.
- Triglycerides > 110 mg/dL (diagnostic).
- Triglycerides 50-110 mg/dL is borderline; requires lipoprotein analysis to confirm chylomicrons.
- Triglycerides < 50 mg/dL makes chylothorax unlikely.
- Pleural fluid cholesterol to triglyceride ratio < 1.
- Imaging: CXR shows pleural effusion. CT chest can help identify the underlying cause (e.g., mediastinal mass, trauma). Lymphangiography (conventional or MR) can localize the leak if needed for intervention.
- Thoracentesis (Gold Std): Pleural fluid analysis is key.
-
DDx (of pleural effusion):
- Pseudochylothorax: Milky appearance but due to high cholesterol (>200 mg/dL) and cholesterol crystals, not triglycerides. Seen in chronic inflammatory effusions like TB or rheumatoid arthritis.
- Empyema: Purulent fluid, high neutrophils, positive culture. Supernatant is clear after centrifugation, unlike chylothorax.
- Hemothorax: Bloody fluid, Hct of fluid is >50% of serum Hct.
- Transudative vs. Exudative effusions: Chylothorax is typically an exudate by Light’s criteria.
-
Management/Treatment:
- Conservative (First-line): Goal is to decrease chyle flow.
- Drainage of pleural fluid (thoracentesis or chest tube) for symptom relief.
- Dietary modification: Total parenteral nutrition (TPN) or a low-fat diet with medium-chain triglyceride (MCT) supplementation (MCTs are absorbed directly into the portal system, bypassing lymphatics).
- Medical: Octreotide/Somatostatin can reduce chyle flow.
- Invasive/Surgical: Indicated for failure of conservative management, high-output fistulas (>1-1.5 L/day), or rapid nutritional decline.
- Thoracic duct ligation (standard surgical approach).
- Thoracic duct embolization (interventional radiology).
- Pleurodesis (chemical or surgical).
- Conservative (First-line): Goal is to decrease chyle flow.
-
Key Associations/Complications:
- Complications: Result from chronic loss of chyle.
- Malnutrition and weight loss (loss of fats, proteins, fat-soluble vitamins).
- Immunosuppression (loss of T-lymphocytes and immunoglobulins), leading to increased infection risk.
- Dehydration and electrolyte abnormalities.
- Associations: Lymphoma, Down syndrome, Noonan syndrome, Turner syndrome.
- Complications: Result from chronic loss of chyle.