- Dizygotic (Fraternal) Twins
- Pathophysiology: Fertilization of 2 separate oocytes by 2 separate sperm.
- Genetics: Siblings sharing ~50% of genetic material.
- Placentation: Always Dichorionic/Diamniotic (Di/Di).
- 2 Placentas (may fuse if close), 2 Chorions, 2 Amnions.
- Epidemiology: Incidence varies (unlike MZ twins).
- Risk Factors:
- ↑ Maternal Age (↑ FSH).
- Assisted Reproductive Technology (ART) (e.g., Clomiphene, IVF).
- Ethnicity (African > Caucasian > Asian).
- Family Hx of twins (maternal lineage).
- Monozygotic (Identical) Twins
- Pathophysiology: Fertilization of 1 oocyte by 1 sperm, followed by cleavage (splitting).
- Genetics: Genetically identical.
- Epidemiology: Incidence is constant worldwide (~1/250). Not influenced by maternal age or hereditary factors.
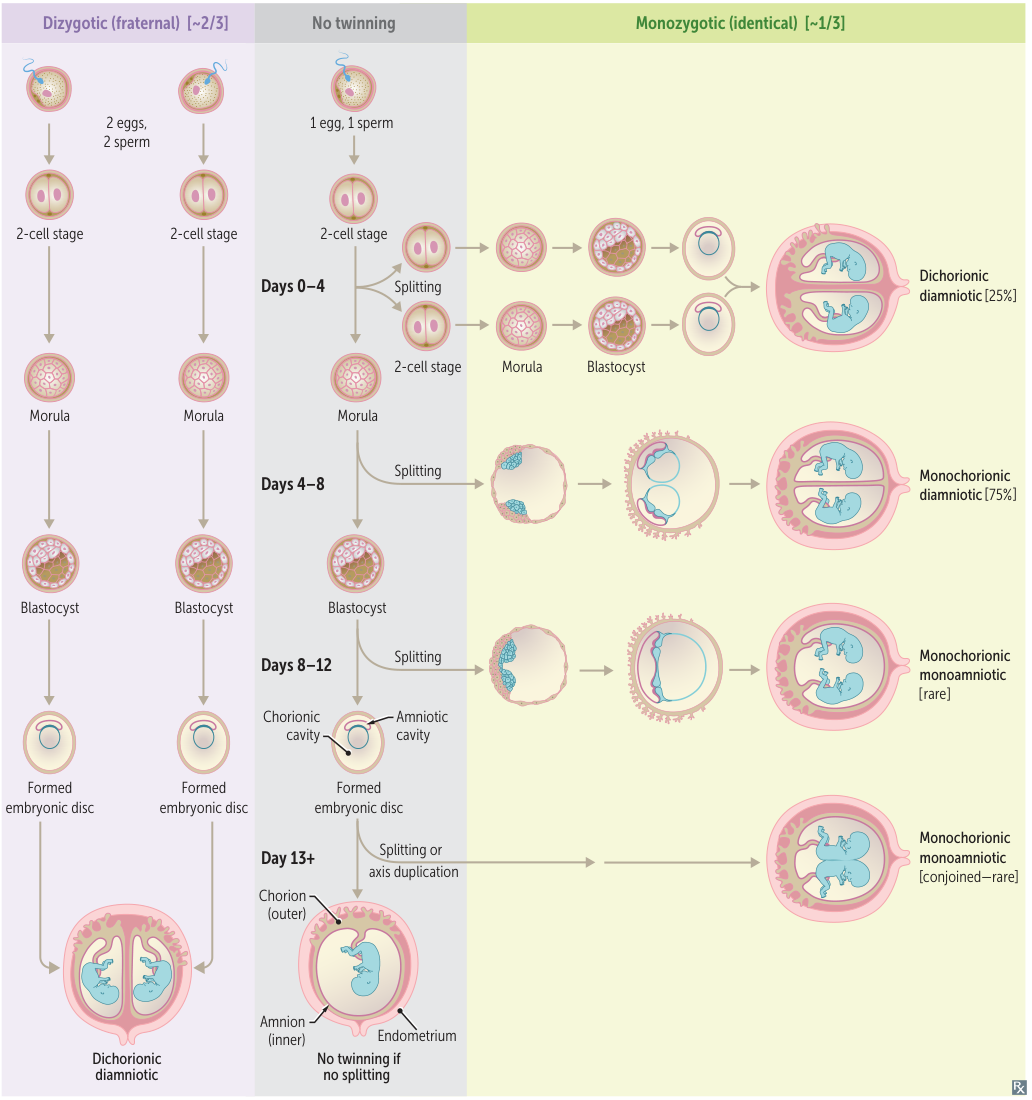
- Placentation (Determined by Timing of Cleavage)
- Fundamental Principle: The chorion (which forms the fetal part of the placenta) develops from the trophectoderm, the outer cell layer of the blastocyst. The amnion develops later from the inner cell mass (epiblast). Therefore, whether these structures are shared depends on whether the split occurs before or after they are formed.
- The later the split, the more structures are shared.
- Mnemonic: SCAB (Separate, Chorion, Amnion, Body)
- Days 0–4 (Cleavage of Morula):
- Dichorionic/Diamniotic (Di/Di) (~25%).
- 2 Placentas, 2 Sacs. Best prognosis.
- Days 4–8 (Cleavage of Blastocyst):
- Monochorionic/Diamniotic (Mo/Di) (~75% - Most Common).
- 1 Placenta, 2 Sacs. Risk of Twin-Twin Transfusion Syndrome (TTTS).
- Days 8–12 (Cleavage of Implanted Blastocyst):
- Monochorionic/Monoamniotic (Mo/Mo) (<1%).
- 1 Placenta, 1 Sac. High risk of cord entanglement.
- Days >13 (Cleavage of Embryonic Disc):
- Conjoined Twins.
- Ultrasound Signs (Chorionicity)
- Lambda (λ) Sign (or Twin Peak sign): Indicates Dichorionic (thick membrane separating twins).
- T-Sign: Indicates Monochorionic (thin membrane separating twins, fusing at a right angle).
- Specific Complications
- Twin-Twin Transfusion Syndrome (TTTS) t
- Mechanism: Unbalanced AV anastomoses in a Monochorionic placenta.
- Donor Twin: Hypovolemia, anemia, oligohydramnios, “stuck twin” appearance, growth restriction.
- Recipient Twin: Hypervolemia, polycythemia, polyhydramnios, cardiomegaly, hydrops fetalis.
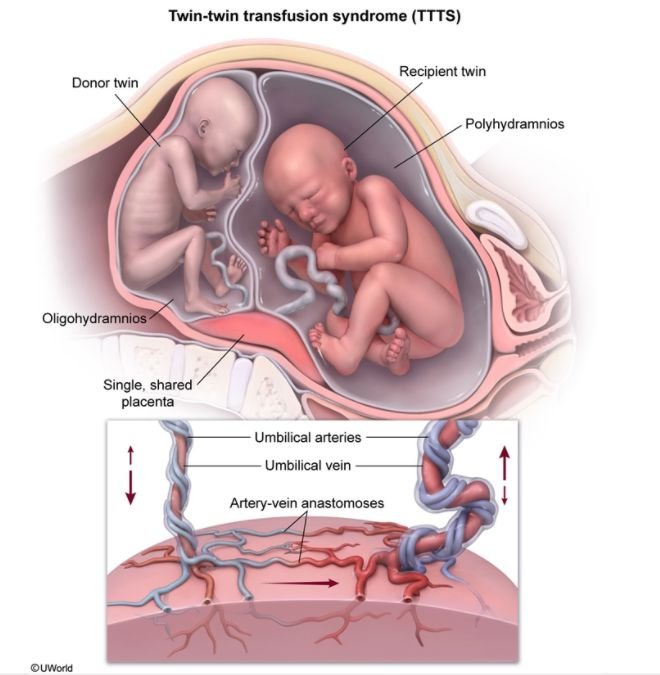
- Tx: Fetoscopic laser ablation of anastomoses.
- Twin Anemia-Polycythemia Sequence (TAPS)
- Similar to TTTS but caused by small AV anastomoses; leads to significant Hgb difference without the amniotic fluid discordance (no oligo/polyhydramnios sequence).
- Cord Entanglement: Specific to Mo/Mo twins.
- Twin Embolization Syndrome: If one twin dies in utero, thromboplastin emboli can damage the surviving twin (renal cortical necrosis, cerebral palsy).
- Twin-Twin Transfusion Syndrome (TTTS) t
- General Multi-Gestation Risks
- Preterm Labor (Most common complication).
- Preeclampsia.
- Postpartum Hemorrhage (uterine atony due to overdistention).
- IUGR (Intrauterine Growth Restriction).
| Identical twins (monozygotic twins) | Fraternal twins (dizygotic twins) | |
|---|---|---|
| Frequency | ⅓ of all twin pregnancies | ⅔ of all twin pregnancies |
| Origin | Division of the fertilized oocyte into two embryonic layers | Fertilization of two oocytes with two mature spermatozoa |
| Genetics of the individual | Genetically identical | Genetically different |
| Chorionic cavity and amniotic sac | Varies (see below) | Dichorionic-diamniotic |
take separate cars or share a CAB
- Splitting 0–4 days: separate chorion and amnion (di-di)
- Splitting 4–8 days: shared Chorion (mo-di)
- Splitting 8–12 days: shared chorion and Amnion (mo-mo)
- Splitting 13+ days: shared chorion, amnion, and Body (mo-mo; conjoined)