Urinary tract cancer most commonly involves the bladder, although it may also occur in the renal pelvis, ureters, and, rarely, the urethra.
Epidemiology
- Cancer sites
- Bladder (90%)
- Renal pelvis and renal calyces (8%)
- Ureter and urethra (2%)
- Histological types
- Transitional cell (urothelial) carcinoma: most common (∼ 95%) type of cancer of the bladder, ureter, renal pelvis, and proximal urethra in male individuals
- Squamous cell carcinoma: most common (∼ 60%) type of cancer of the distal urethra in male individuals and the entire urethra in female individuals
- Risk Factors (Pee SAC):
- Phenacetin (obsolete analgesic)
- Smoking (#1 risk factor, polycyclic aromatic hydrocarbons) t
- Aromatic amines (aniline dyes; rubber, plastic, textile industries)
- Cyclophosphamide (causes hemorrhagic cystitis → ↑ risk)
- Schistosoma haematobium: Associated with Squamous Cell Carcinoma of the bladder, not urothelial t
Pathogenesis
- Two distinct pathways:
- Papillary pathway: Low grade → High grade → Invasion. Not associated with early p53 mutations.
- Flat pathway: High grade (Carcinoma in situ/CIS) → Invasion. Associated with early p53 mutations.
- Field Cancerization: Entire urothelium is exposed to carcinogens, leading to multifocal tumors and high recurrence rates.
Pathology
- Papillary urothelial carcinoma
- A thick papilla with a fibrovascular core
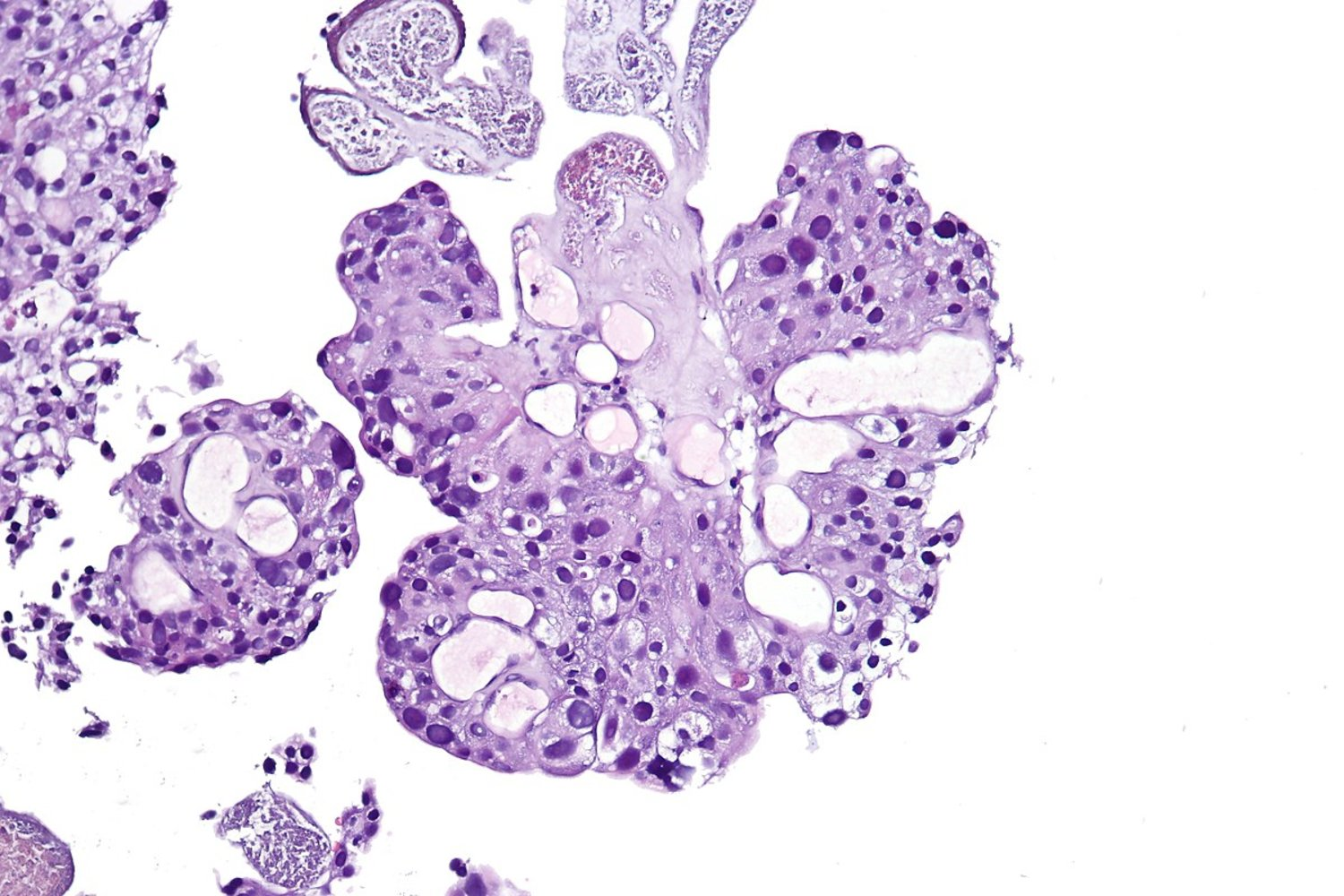
- A thick papilla with a fibrovascular core
- Squamous cell carcinoma
- Chronic inflammatory stimuli (e.g., schistosomiasis, chronic cystitis) can lead to transformation of urothelial cells into squamous epithelial cells (squamous metaplasia)